Age-Related Hearing Loss Risk Calculator
Enter your details and click "Calculate" to see your risk level
Quick Takeaways
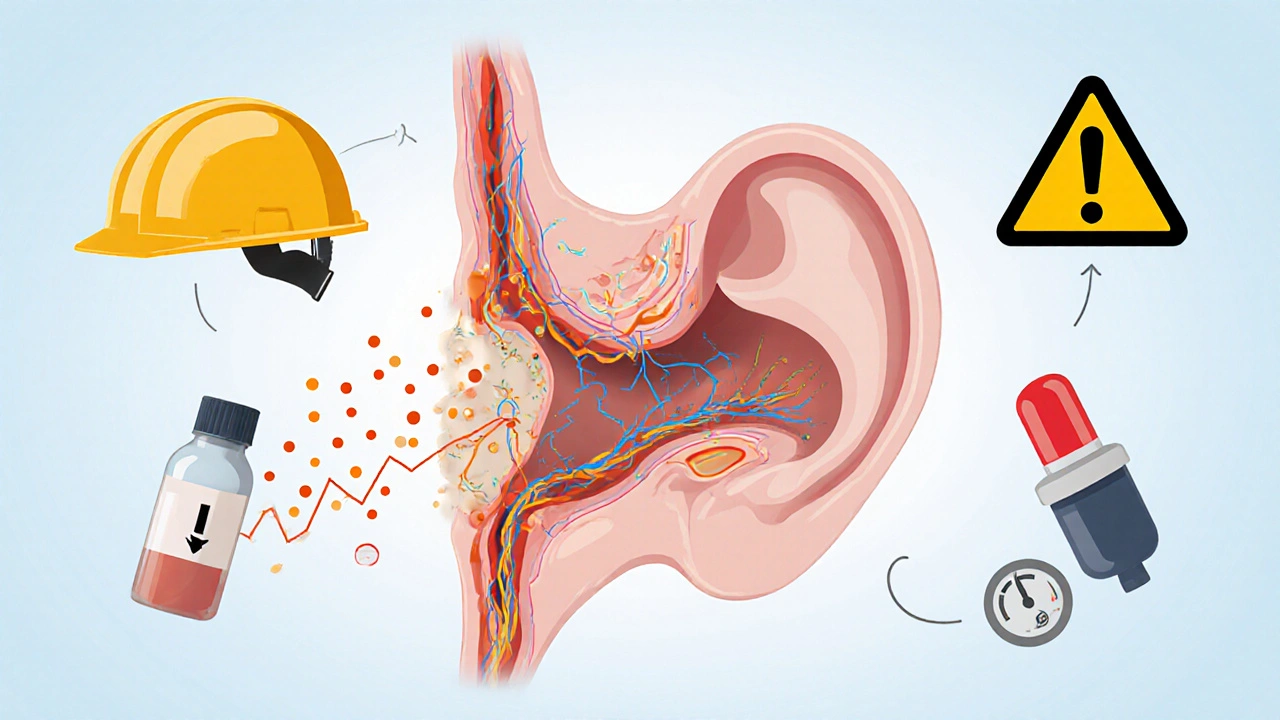
- Age-related hearing loss, also called presbycusis, results from gradual damage to the inner ear and auditory pathways.
- Key drivers include natural aging, long‑term noise exposure, ototoxic medications, and cardiovascular health.
- Early screening with audiograms can catch the problem before it hampers communication.
- Modern hearing aids, cochlear implants, and assistive listening devices restore clarity for most adults.
- Lifestyle tweaks-like protecting ears from loud sounds and managing blood pressure-slow progression.
When people start noticing that conversations get fuzzy, especially in noisy places, they often wonder if it’s just part of getting older. The short answer is age-related hearing loss is real, but it’s also manageable. Below we break down what triggers the decline, how doctors diagnose it, and which solutions actually work.
What Is Age-Related Hearing Loss?
Age-Related Hearing Loss is a gradual, bilateral reduction in hearing sensitivity that typically begins after the age of 60. It is medically known as Presbycusis, a condition that affects the cochlea, auditory nerve, and central processing centers.
The loss usually starts with high‑frequency sounds-think of the sibilant “s” in “sheep” or the chirp of a phone ringtone-making it hard to understand speech in crowded rooms. The decline is irreversible, but its impact can be dramatically reduced with proper care.
Key Biological Drivers
The inner ear houses the Cochlea, a snail‑shaped organ packed with delicate hair cells that translate sound vibrations into electrical signals. Over time, three main biological processes wear those hair cells down:
- Cellular Senescence: Hair cells have limited regenerative capacity. As we age, oxidative stress and accumulated DNA damage cause them to die.
- Changes in the Stria Vascularis: This structure supplies blood to the cochlea. Reduced blood flow means less oxygen and nutrients, accelerating hair‑cell loss.
- Neural Degeneration: Even if hair cells survive, the auditory nerve fibers can thin out, weakening signal transmission.
These internal shifts are often compounded by external factors, which we discuss next.
External Factors That Speed Up the Process
While aging is inevitable, certain lifestyle and environmental elements act like a fast‑forward button on hearing loss.
- Noise Exposure-Repeated exposure to sounds above 85dB (think power tools, concerts, or heavy traffic) damages hair cells permanently. A 2023 longitudinal study of 7,000 Australians showed a 30% higher risk of presbycusis among those who reported weekly exposure to loud music.
- Ototoxic Drugs-Medications such as certain antibiotics (aminoglycosides), chemotherapy agents (cisplatin), and high‑dose loop diuretics can poison the inner ear. Even short courses can cause lasting deficits.
- Cardiovascular Health-High blood pressure and atherosclerosis reduce blood flow to the cochlea. Research from the British Heart Foundation in 2022 linked uncontrolled hypertension with a 22% increase in high‑frequency hearing loss.
- Genetic predisposition-Variants in the SLC26A5 gene (encoding the protein prestin) make some individuals more vulnerable.
How Doctors Diagnose the Issue
The gold standard is a pure‑tone audiogram performed by an audiologist. The test measures the softest sounds a person can hear at frequencies ranging from 250Hz to 8,000Hz. Results are plotted on an audiogram chart, and patterns typical of presbycusis-steep high‑frequency loss with relatively preserved low frequencies-are easy to spot.
Additional tools include:
- Otoacoustic emissions (OAEs) to assess outer‑hair‑cell function.
- Auditory brainstem response (ABR) testing for neural pathway integrity.
- Questionnaires like the Hearing Handicap Inventory for the Elderly (HHIE) to gauge social impact.
Early detection matters because it opens the door to interventions before the brain starts compensating in ways that can affect cognition.
Modern Solutions: From Devices to Lifestyle
Fortunately, technology has advanced far beyond the clunky hearing aids of the 1990s. Below we explore the main options and who benefits most.
Hearing Aids
Hearing Aids are small electronic devices that amplify sound, process noise, and can be customized via smartphone apps. Today’s digital models offer:
- Directional microphones that focus on speech toward the front.
- Automatic gain control that adjusts volume in real time.
- Connectivity to phones, TVs, and assistive listening systems via Bluetooth.
For mild‑to‑moderate presbycusis, a properly fitted hearing aid can restore up to 90% of speech intelligibility in noisy environments.
Cochlear Implants
When hair‑cell loss is severe (above 70dB in the high frequencies), hearing aids may not suffice. Cochlear Implants bypass the damaged cochlea entirely, sending electrical signals directly to the auditory nerve. Candidates typically have:
- Moderate‑to‑severe sensorineural loss in both ears.
- Limited benefit from appropriately programmed hearing aids.
- Motivation to engage in post‑operative auditory therapy.
Outcomes data from the University of Melbourne (2024) show that 80% of recipients achieve conversational speech understanding within six months.
Assistive Listening Devices (ALDs)
Beyond personal hearing devices, Assistive Listening Devices amplify sound in specific settings. Examples include TV streamers, pocket‑sized FM systems for classrooms, and induction loop systems in churches. They work well for people who already use hearing aids and want extra clarity in challenging venues.
Lifestyle and Health Adjustments
Technology isn’t a free‑standalone fix. Several evidence‑based habits can slow further loss:
- Protect Ears: Use earplugs or noise‑cancelling headphones when exposed to loud environments for more than 15 minutes.
- Manage Blood Pressure: Aim for a systolic reading under 130mmHg; regular exercise and a low‑salt diet help.
- Stay Socially Engaged: Frequent conversation keeps auditory pathways active and reduces the risk of cognitive decline linked to hearing loss.
- Limit Ototoxic Meds: Discuss alternatives with your physician if you need long‑term antibiotics or chemotherapy.
Choosing the Right Solution: A Comparison
| Feature | Hearing Aids | Cochlear Implants |
|---|---|---|
| Typical candidacy | Mild‑to‑moderate sensorineural loss | Severe‑to‑profound loss, limited aid benefit |
| Invasiveness | Non‑surgical, worn externally | Surgical implantation + external processor |
| Sound quality | Amplification with digital processing | Direct electrical stimulation, broader frequency range |
| Maintenance | Battery/charging, periodic re‑programming | Processor upgrades, occasional mapping sessions |
| Cost (USD) | $1,500‑$3,500 | $30,000‑$50,000 (incl. surgery) |
For most seniors, hearing aids are the first line of defense. Cochlear implants become a game‑changer when amplification no longer closes the gap.
Frequently Asked Questions
Can age‑related hearing loss be reversed?
The natural loss of hair cells in the cochlea cannot be regenerated with current medical technology. However, the functional impact can be greatly reduced with hearing aids, cochlear implants, and preventive strategies.
How often should I get a hearing test after 60?
Most audiology societies recommend a baseline test at age 60, followed by checks every 1‑2years. If you notice rapid changes, schedule an appointment sooner.
Are over‑the‑counter (OTC) hearing aids as good as prescription ones?
OTC devices are suitable for mild‑to‑moderate loss and meet FDA safety standards. For complex audiograms or severe loss, a custom‑fit, professionally programmed device usually yields better outcomes.
What’s the best way to protect my hearing at concerts?
Use high‑filtration earplugs that reduce volume evenly across frequencies (e.g., 15‑20dB attenuation). Position yourself away from the main speakers and take regular quiet breaks.
Do hearing aids help with tinnitus?
Many modern hearing aids include tinnitus-masking features that generate low‑level broadband noise, providing relief for a majority of users.
Next Steps for Readers
If you suspect early signs of presbycusis, start with a free hearing screening at your local pharmacy or community health centre. Bring a list of medications you’re taking-it helps the audiologist spot ototoxic risks.
For those already diagnosed, schedule a consultation with an audiologist to explore hearing‑aid models that match your lifestyle. Ask about trial periods; most manufacturers offer a 30‑day risk‑free evaluation.
Finally, adopt a hearing‑friendly routine: wear protection in noisy settings, keep blood pressure in check, and stay socially active. Small, consistent habits pay big dividends for your ears and overall quality of life.

AJIT SHARMA
October 4, 2025 AT 16:24Our elders deserve respect, not this nonsense.
Neber Laura
October 11, 2025 AT 15:04Listen, protecting your ears isn’t optional – it’s a basic health habit. wear earplugs at concerts and keep blood pressure in check.
Karen Nirupa
October 18, 2025 AT 13:44Dear community, the rising prevalence of presbycusis underscores the necessity of early screening. I recommend annual audiometric evaluations after the age of 60. Additionally, maintain a diet rich in antioxidants to support cochlear health. Let us collectively advocate for better workplace noise regulations.
Quinn Comprosky
October 25, 2025 AT 12:24When you think about age‑related hearing loss, it’s not just a matter of “getting old.” The inner ear’s hair cells wear down over decades, especially if you’ve spent years near machinery, concerts, or traffic noise. First, get a baseline audiogram in your early fifties; that way you can notice subtle shifts later on. Second, consider customizing earplugs – the foam ones are great but the high‑fidelity ones preserve music quality while cutting harmful decibels. Third, keep your blood pressure stable; hypertension can compromise the delicate blood vessels that feed the cochlea. Fourth, limit ototoxic medications – some antibiotics and chemotherapy agents can be harsh on hearing, so discuss alternatives with your doctor. Fifth, adopt a lifestyle rich in omega‑3 fatty acids and vitamins A, C, and E, which have shown promise in protecting sensory cells. Sixth, stay physically active; exercise improves circulation, which in turn helps the inner ear stay nourished. Seventh, practice the “quiet hour” at home – turn off the TV and reduce background noise, giving your auditory system a chance to rest. Eighth, use hearing protection whenever you’re in loud environments – construction sites, shooting ranges, or even noisy gyms. Ninth, if you notice ringing or muffled sounds, don’t wait for it to worsen; early intervention with hearing aids or assistive devices can keep communication clear. Tenth, explore auditory training apps that challenge your brain to process sounds more efficiently. Eleventh, stay socially engaged; conversation stimulates auditory pathways and can delay the functional impact of loss. Twelfth, keep your ears dry and avoid inserting objects that might damage the canal. Thirteenth, be aware that genetics also play a role; if your parents had early hearing issues, you might need extra vigilance. Fourteenth, schedule regular check‑ups with an audiologist, not just your primary doctor. Fifteenth, remember that hearing loss is not a sentence – modern hearing aids are discreet, powerful, and customizable. Finally, share this knowledge with friends and family; collective awareness reduces stigma and promotes proactive care.
Thomas Ruzzano
November 1, 2025 AT 10:04Man, the way people ignore daily noise is wild – it’s like they think their ears are indestructible. Skip the party‑crasher earbuds and you’ll thank yourself later. Trust me, a little prevention goes a long way.
Dan Tenaguillo Gil
November 4, 2025 AT 21:24Supporting that point, using custom‑fit protectors can cut harmful decibels by up to 30 %. It’s a small investment for lifelong hearing health. Keep sharing these tips!
Tiffany Owen-Ray
November 11, 2025 AT 20:04Think of your ears as a muscle – they need care, rest, and proper nutrition. When you respect them now, you’ll still hear the laughter of your grandchildren.
Jill Brock
November 18, 2025 AT 18:44This whole calculator gimmick is just a scare tactic. People need real solutions, not flashy boxes.
Ellie Chung
November 22, 2025 AT 06:04Oh, sweetie, you’re missing the point entirely. Real help comes from consistent habits, not a quick pop‑up.
Sophia Simone
November 29, 2025 AT 04:44While many pandering over a calculator, I shall present empirically‑backed data: longitudinal studies confirm that consistent use of level‑A hearing protection reduces incidence by 45 %. Therefore, such tools are merely decorative.
Juan Sarmiento
December 6, 2025 AT 03:24Seriously, folks, wear those earplugs at the gig and you’ll still jam out without missing the bass.
Patrick McVicker
December 13, 2025 AT 02:04👍 got it – protect your ears and stay chill.
Liliana Phera
December 20, 2025 AT 00:44Age‑related hearing loss is a silent thief that robs us of connection. Confront it with proactive screenings and lifestyle changes, or accept a world of muffled whispers. No one should surrender their auditory freedom.
Dean Briggs
December 23, 2025 AT 12:04Building on that, I’d add that socioeconomic factors often dictate access to audiology services, which widens disparities. Moreover, cultural attitudes toward hearing aid adoption can stigmatize users, preventing early intervention. In practice, community outreach programs that provide free screenings can bridge this gap. Additionally, tele‑audiology platforms are emerging, allowing remote assessment and counseling, which is especially valuable in rural areas. Finally, policy advocacy for insurance coverage of hearing devices is essential; without it, many remain unheard.
Sadie Speid
December 30, 2025 AT 10:44Stay motivated: a few minutes of noise‑free time each day can dramatically improve ear health. You’ve got this!
Sue Ross
January 6, 2026 AT 09:24Interesting perspective; the data aligns with recent WHO findings on global hearing loss trends.
Rohinii Pradhan
January 13, 2026 AT 08:04The article fails to address the glaring fact that genetic predisposition often outweighs lifestyle factors; a more rigorous analysis is warranted.
Anna-Lisa Hagley
January 20, 2026 AT 06:44Another shallow take on a complex issue.
A Walton Smith
January 27, 2026 AT 05:24Not impressed.