Menopause Urinary Incontinence Risk Assessment
Assessment Guide
Answer the following questions to assess your risk for menopause-related urinary incontinence.
When women hit the menopause milestone, many expect hot flashes or sleep changes, but menopause urinary incontinence often slips under the radar. Suddenly, a sudden urge to pee, leaks during a laugh, or a constant feeling of wetness can feel embarrassing and disruptive. The good news? Understanding why it happens and what you can do about it puts you back in control.
Key Takeaways
- Estrogen loss during menopause weakens the pelvic floor and thins the lining of the urethra, making leaks more likely.
- Lifestyle tweaks-fluid timing, weight control, and targeted Kegel exercises-help many women manage symptoms without medication.
- Hormone therapy, prescription meds, and minimally invasive procedures are effective options if home strategies aren’t enough.
- Early assessment (a symptom diary and a quick pelvic exam) speeds up the right treatment plan.
- A simple prevention checklist can keep symptoms at bay long after menopause ends.
Menopause is the natural cessation of ovarian hormone production, usually occurring between ages 45 and 55. During this transition, the body’s estrogen and progesterone levels drop dramatically, triggering a cascade of changes throughout the urinary tract.
Urinary Incontinence is the involuntary loss of urine, ranging from occasional dribbles to frequent, disruptive leaks. In post‑menopausal women, the most common types are stress incontinence (leakage during coughing, sneezing, or exercise) and urge incontinence (a sudden, intense need to void).
How Menopause Affects the Urinary System
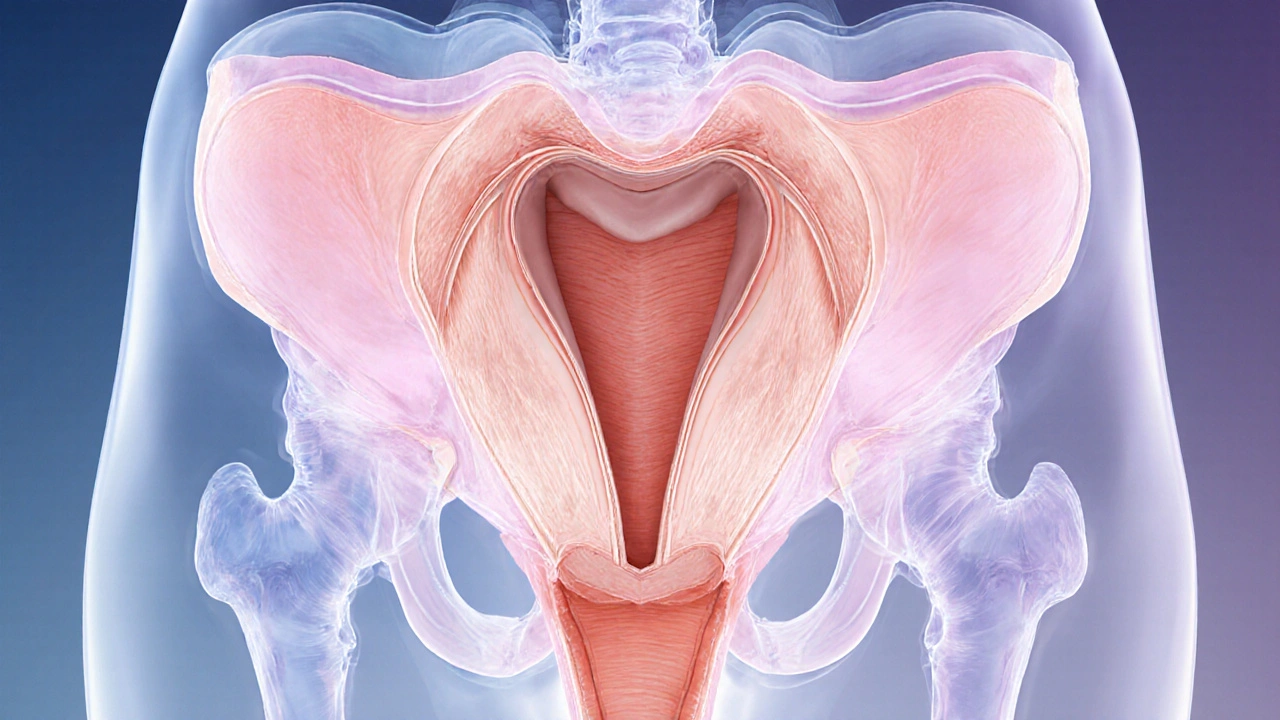
The urinary system comprises the kidneys, ureters, bladder, and urethra. While the kidneys and ureters remain largely untouched by hormonal shifts, the bladder and urethra are hormone‑sensitive. Declining estrogen leads to three key changes:
- Urethral lining thinning: Less estrogen means a thinner, less elastic urethral wall, reducing its ability to stay closed under pressure.
- Reduced pelvic floor muscle tone: The Pelvic Floor Muscle is a group of muscles that support the bladder, uterus, and bowel loses strength, making it harder to control urine flow.
- Vaginal and urethral tissue atrophy: Known as Vaginal Atrophy is the thinning and drying of the vaginal walls due to low estrogen, which also affects the urethra and contributes to irritation and urgency.
These physiological shifts explain why many women notice a new pattern of leaks within the first few years after their periods stop.
Common Triggers and Risk Factors
Beyond hormonal changes, several lifestyle and health factors amplify leakage risk:
- Body weight: Excess abdominal pressure strains the pelvic floor.
- Chronic coughing or constipation: Repeated pressure spikes weaken support structures.
- Smoking: Damages connective tissue and irritates the bladder.
- Caffeine and alcohol: Both act as diuretics, increasing urine volume and urgency.
- Medications: Some antihistamines, antidepressants, and diuretics can trigger overactive bladder symptoms.
Assessing Your Symptoms
Before jumping to treatments, a quick self‑assessment helps pinpoint the type and severity of leakage.
- Keep a 3‑day bladder diary: note fluid intake, times you urinate, any leaks, and activities at the moment.
- Rate the frequency on a scale of 0-5 (0=none, 5=daily multiple episodes).
- Schedule a brief exam with your primary care provider or a urogynecologist. They’ll likely perform a simple cough stress test and a quick pelvic floor muscle evaluation.
If your score is 3 or higher, or if leaks interfere with work or social life, it’s time to explore targeted solutions.
Home and Lifestyle Strategies
Many women find relief by tweaking daily habits and strengthening the pelvic floor.
Fluid Management
- Spread fluid intake evenly throughout the day-avoid loading up in the evening.
- Limit caffeine to one cup and alcohol to one standard drink per day.
- Choose water, herbal teas, and diluted fruit juices over sodas.
Weight and Core Health
- Aim for a BMI under 25; even a 5‑% weight loss can improve leak frequency.
- Incorporate low‑impact cardio (walking, swimming) and core‑stabilizing exercises (planks, bridges).
Kegel Exercise Program
The Kegel Exercise is a pelvic floor contraction technique that strengthens the muscles supporting the bladder and urethra. Here’s a simple starter routine:
- Locate the right muscles: stop urine flow mid‑stream once-those are your pelvic floor muscles.
- Contract for 5 seconds, then relax for 5 seconds. Aim for 10 repetitions.
- Do three sets daily. Gradually increase hold time to 10 seconds.
Consistency is key. Most studies show noticeable improvement after 6‑8 weeks of regular practice.
Bladder Training
- Start with a 2‑hour interval between bathroom trips, then slowly stretch to 3‑4 hours.
- If urgency hits, use “quick‑squeeze” Kegels before you go to help the bladder empty fully.
Medical and Hormonal Options
When lifestyle fixes aren’t enough, several evidence‑based medical avenues exist.
Estrogen Therapy
Localized estrogen (creams, rings, or tablets) directly nourishes the urethral and vaginal tissues, often restoring normal closure pressure.
- Typical dosage: low‑dose estradiol cream applied to the vaginal vestibule two times weekly.
- Benefits appear within 2-4 weeks; side effects are rare when used locally.
Systemic hormone replacement therapy can also help, but it’s usually reserved for women needing relief from broader menopausal symptoms.
Prescription Medications
- Mirabegron: a β3‑adrenergic agonist that relaxes the bladder muscle, reducing urgency.
- Antimuscarinics (e.g., oxybutynin): calm overactive bladder contractions but may cause dry mouth.
Doctors often start with the lowest effective dose and adjust based on tolerance.
Pelvic Floor Physical Therapy
Specialized therapists use biofeedback, electrical stimulation, and manual techniques to retrain the Pelvic Floor Muscle more effectively than home Kegels alone.
- Typical course: 6-8 weekly sessions, plus a home program.
- Success rates of 60‑80% for stress incontinence.
Minimally Invasive Procedures
- Urethral bulking agents: injectable silicone‑based material adds bulk to the urethra, improving closure.
- Botox injections: relax overactive bladder muscles, lowering urgency episodes.
- Both procedures are office‑based, with downtime of 1-2 days.
Surgical Options
For persistent stress incontinence, sling procedures (mid‑urethral slings) provide high cure rates (≈90%). Surgery is usually considered after conservative measures fail for at least a year.

Choosing the Right Path: A Quick Comparison
| Option | Efficacy | Invasiveness | Typical Cost (US$) | Common Side Effects |
|---|---|---|---|---|
| Lifestyle & Kegels | Moderate (30‑60% improvement) | None | 0‑200 | None |
| Pelvic Floor PT | High (60‑80% improvement) | None | 200‑600 | Muscle soreness |
| Local Estrogen | High (40‑70% reduction) | Minimal | 50‑150 per month | Vaginal irritation |
| Prescription Meds | Moderate‑high | Oral/Transdermal | 100‑300 | Dry mouth, constipation |
| Bulking Agents / Botox | High (70‑85% relief) | Minor procedure | 600‑1300 | Urinary retention (rare) |
| Sling Surgery | Very high (≈90% cure) | Surgical | 3000‑8000 | Pain, infection |
Prevention Checklist
- Stay active-aim for at least 150 minutes of moderate exercise per week.
- Practice Kegels daily, gradually increasing hold time.
- Maintain a healthy weight; waist circumference under 35inches is a good target.
- Limit caffeine, alcohol, and carbonated drinks.
- Quit smoking-each pack‑year adds pressure on pelvic tissues.
- Schedule a yearly pelvic health check after menopause.
Frequently Asked Questions
Is urinary incontinence a normal part of aging?
Leakage becomes more common after menopause, but it isn’t inevitable. Hormonal changes, lifestyle, and pelvic floor health all play roles, and many women regain control with simple interventions.
Can hormone therapy worsen other health issues?
Systemic hormone therapy carries risks for heart disease and certain cancers, so doctors weigh benefits against personal history. Local estrogen applied to the vagina or urethra has far fewer systemic effects and is generally safe for bladder symptoms.
How long does it take to see results from Kegel exercises?
Most research shows measurable improvement after 6‑8 weeks of daily practice. Consistency matters-skipping days can set progress back.
Should I wear pads all day?
Pads can protect clothing, but they don’t treat the cause. Use them sparingly while you work on underlying solutions like pelvic floor strengthening or medical therapy.
When is surgery the right choice?
Surgery is usually considered when leaks persist daily despite at least a year of conservative treatment, and when quality‑of‑life impact is high. A urogynecologist can evaluate sling options and discuss risks.

Jagdish Kumar
October 5, 2025 AT 23:33It is rather astonishing how the decline in estrogen during menopause orchestrates a cascade of physiological alterations, particularly within the lower urinary tract. The attenuation of urethral mucosal coaptation, coupled with diminished collagen synthesis, predisposes many women to stress urinary incontinence. Moreover, the concomitant increase in adipose tissue exacerbates intra‑abdominal pressure, further compromising sphincteric competence. A comprehensive assessment, therefore, must extend beyond mere symptomatology to encompass hormonal and biomechanical determinants.
Aminat OT
October 6, 2025 AT 00:33omg i feel u lol this whole thing hits hard, i’ve been crying at night cuz i can’t even get up to the bathroom without feeling embarrassed 😭
Amanda Turnbo
October 6, 2025 AT 01:33Honestly, the article glosses over the role of pelvic floor physiotherapy, which is arguably the most evidence‑based non‑surgical intervention. Skipping that discussion feels like a lazy afterthought.
Jenn Zuccolo
October 6, 2025 AT 02:33One might contemplate the existential dimension of bodily change: menopause invites a renegotiation of identity, wherein the bladder becomes a metaphor for loss of control. By framing urinary incontinence within this philosophical tapestry, we appreciate not merely the mechanical dysfunction but also the psychological reverberations that accompany it.
Courtney The Explorer
October 6, 2025 AT 03:33From a biomechanical lens, the interplay of pelvic floor tensile stress and intra‑abdominal pressure gradient constitutes a critical vector; neglecting this vector in therapeutic algorithms undermines efficacy.
Ashleigh Connell
October 6, 2025 AT 04:33I totally get how overwhelming this can feel, and it’s important to remember that lifestyle tweaks-like mindful hydration timing and low‑impact core strengthening-can make a genuine difference without feeling like a medical nightmare.
Erin Knight
October 6, 2025 AT 05:33Well, that’s just basic physiology, nothing groundbreaking.
Kavita Jadhav
October 6, 2025 AT 06:33It’s true that the mechanisms are well‑documented, yet for many women the lived experience of leakage carries a heavy emotional burden. Empathy and validation go a long way; acknowledging the frustration can empower patients to seek the multimodal interventions that truly help.
Tony Halstead
October 6, 2025 AT 07:33Menopause heralds a complex endocrine transition that reverberates across multiple organ systems, and the lower urinary tract is no exception.
As ovarian estrogen production wanes, the urethral epithelium undergoes atrophic changes that diminish its intrinsic closure pressure.
Concurrently, the levator ani and pubococcygeus muscles, which constitute the primary support for the bladder neck, frequently lose tone and strength.
These neuro‑muscular alterations are compounded by systemic factors such as increased central obesity, which elevates intra‑abdominal pressure during routine activities.
Moreover, chronic comorbidities like cough, constipation, and smoking further stress the continence mechanism, creating a perfect storm for leakage.
Epidemiological data indicate that up to 50 % of post‑menopausal women report some degree of urinary incontinence, yet the condition remains under‑reported due to stigma.
The first step in management is a thorough risk assessment, including quantification of leakage episodes, urgency patterns, and lifestyle contributors.
Pelvic floor muscle training, guided by a qualified physiotherapist, has been shown to reduce symptom severity in up to 70 % of participants.
For those with predominant stress incontinence, minimally invasive sling procedures offer high cure rates with relatively low morbidity.
Pharmacologic options, such as topical estrogen creams, can restore urethral mucosal health, while anticholinergic agents target urgency‑dominant presentations.
It is essential to adopt a personalized, multidisciplinary approach that respects the patient’s preferences, cultural context, and comorbid conditions.
Education about fluid management-avoiding excessive caffeine and timing fluid intake-can prevent nocturnal urgency without compromising hydration.
Weight loss, even modestly, reduces intra‑abdominal pressure and improves overall pelvic floor function.
Finally, ongoing research into regenerative therapies and neuromodulation holds promise for future generations of women navigating menopause.
By integrating these evidence‑based strategies, clinicians can transform a potentially debilitating symptom into a manageable aspect of aging.
leo dwi putra
October 6, 2025 AT 08:33Wow, that was a marathon lecture-thanks for the deep dive, but I’m just looking for quick relief!