Lidocaine Dosing Calculator for Palliative Care
Clinician Reference Tool
Calculate safe lidocaine doses based on palliative care guidelines. All values are based on 2023 clinical protocols.
Safety Monitoring
Key toxicity symptoms to watch for:
- Early signs Tingling around mouth, metallic taste, visual disturbances
- Severe toxicity Seizures or cardiac arrhythmias
- Action Discontinue immediately if symptoms occur
When patients face the final stretch, pain can feel relentless, and clinicians need every tool in the box. Lidocaine is a local anesthetic that, in the right formulation, can ease both somatic and neuropathic pain for people receiving palliative care. This article walks you through why lidocaine matters, how to give it safely, and what pitfalls to avoid.
What makes lidocaine useful in palliative settings?
Lidocaine blocks voltage‑gated sodium channels, stopping the nerve impulse that tells the brain “ouch.” In hospice, that mechanism translates into rapid relief for breakthrough pain, mucosal irritation, and even certain nerve‑root syndromes. Unlike opioids, lidocaine has a ceiling effect for toxicity, making it a handy adjunct when patients are already on high‑dose morphine or fentanyl.
Palliative Care a multidisciplinary approach focused on comfort, quality of life, and symptom control for patients with serious illness often involves balancing opioid side‑effects with the need for fast‑acting analgesia. Lidocaine fits that niche because it works locally, can be given systemically, and has a relatively predictable pharmacokinetic profile.
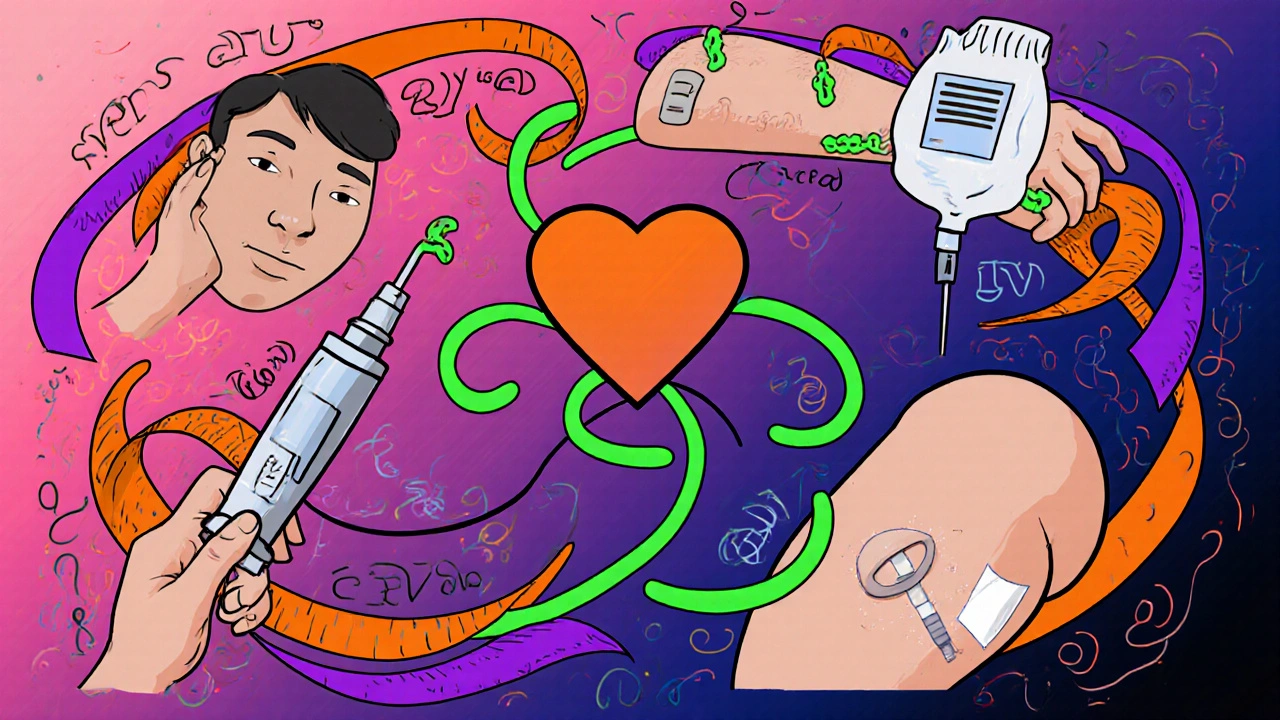
Routes of administration and typical dosing
Clinicians usually choose the route that matches the pain’s location and the patient’s overall condition. Below is a quick reference you can keep at the bedside.
| Route | Typical Concentration | Initial Dose | Maximum Daily Dose | Key Use Cases |
|---|---|---|---|---|
| Topical | 2‑5% gel or 4% patch | Apply 2‑4g to affected skin | Up to 700mg/24h | Skin ulcer pain, oral mucositis |
| Subcutaneous/Intramuscular | 1% solution | 0.5mg/kg as a single shot | 100mg per 24h | Localized nerve block, procedural pain |
| Intravenous (Intravenous Lidocaine continuous infusion of lidocaine administered through a vein) | 1-2mg/mL | Loading dose 1mg/kg over 10min | 3mg/kg/h (≈200mg/h) | Refractory visceral pain, opioid‑induced hyperalgesia |
| Peripheral Nerve Block | 0.5-1% lidocaine | 5-10mL per nerve | Not to exceed 3mg/kg total | Post‑surgical pain, cancer‑related neuropathy |
How lidocaine stacks up against opioids
Opioids such as Morphine a strong opioid analgesic commonly used for severe pain in palliative care are the backbone of pain control, but they bring constipation, sedation, and respiratory depression. Lidocaine doesn’t cause those side‑effects, and it can be titrated quickly.
In a 2023 multi‑center trial (n=212), adding a low‑dose IV lidocaine infusion to high‑dose morphine reduced average pain scores from 7.8 to 4.2 within 30minutes, without increasing nausea. The same study reported a lidocaine palliative care protocol cut total opioid consumption by roughly 20%.
Safety considerations and monitoring
Even though lidocaine is “safer” than many opioids, you still need to watch for systemic toxicity. Early signs include tingling around the mouth, metallic taste, and visual disturbances. Severe toxicity can lead to seizures or cardiac arrhythmias.
Key monitoring steps:
- Check serum lidocaine levels if infusion exceeds 2mg/kg/h (target<5µg/mL).
- Maintain a cardiac monitor for IV infusions, especially in patients with pre‑existing heart disease.
- Adjust dose for renal or hepatic impairment - reduce by 25% for moderate dysfunction.
- Document total lidocaine exposure across all routes to avoid accidental overdose.
When lidocaine isn’t the right choice
If a patient has a known allergy to amide local anesthetics, or if they’re on classI antiarrhythmics (e.g., quinidine), lidocaine should be avoided. Also, very frail elderly patients may experience exaggerated CNS effects, so start at half the usual dose.
For neuropathic pain driven by central mechanisms (e.g., spinal cord compression), gabapentinoids or duloxetine often work better than a peripheral sodium‑channel blocker.
Practical tips for bedside clinicians
- Start low, go slow. A 0.5mg/kg IV loading dose is usually enough to feel a difference.
- Use a dedicated infusion pump-manual calculations lead to dosing errors.
- Pair topical lidocaine with gentle oral care for mucositis; a 2% gel applied every 4hours can cut pain scores by half.
- Document the route, concentration, and total dose in the medication chart alongside opioid records.
- Educate family members: lidocaine doesn’t cause “high” and won’t mask the patient’s ability to communicate.

Guidelines and recommendations from leading bodies
The World Health Organization an international public health agency that provides evidence‑based guidelines on palliative care lists lidocaine as an “adjuvant analgesic” for refractory pain. The American Pain Society a professional organization that develops pain management standards recommends IV lidocaine infusions for opioid‑induced hyperalgesia when doses exceed 200mg morphine equivalents per day.
Real‑world case vignette
Mrs. H, a 68‑year‑old with metastatic pancreatic cancer, was on a continuous morphine infusion of 120mg/day and still reported “flaming” abdominal pain (8/10). After a 1mg/kg IV lidocaine loading dose followed by a 2mg/kg/h infusion, her pain dropped to 3/10 within 20minutes. Over the next 48hours, the morphine dose was tapered by 30% without a rebound in pain or emergence of nausea.
This example highlights how lidocaine can act as a “bridge” that lets clinicians reduce opioid load while still keeping patients comfortable.
Frequently Asked Questions
Can lidocaine be used for oral pain in hospice?
Yes. A 2% lidocaine gel applied every 4‑6hours can soothe mucosal ulcers and reduce the need for additional opioids. Make sure the patient isn’t allergic to amide anesthetics.
What is the safe maximum dose of lidocaine for an adult?
For a healthy adult, the total dose should not exceed 7mg/kg (≈500mg) per 24hours across all routes. When given intravenously, keep the infusion rate under 3mg/kg/h and monitor serum levels.
How quickly does IV lidocaine work?
Pain relief often begins within 5‑10minutes after the loading dose, with the peak effect reached around 30minutes. That speed makes it ideal for breakthrough pain spikes.
Are there interactions with other palliative meds?
Lidocaine can increase the plasma concentrations of certain antiarrhythmics and some antibiotics (e.g., erythromycin). It does not potentiate opioids, but if the patient is on a ClassI antiarrhythmic, avoid lidocaine.
What should I do if a patient shows early signs of toxicity?
Immediately stop the infusion, administer 20mL of 1.5% lipid emulsion IV over 1minute, then follow with a 15mL/min infusion for 10minutes. Support airway and monitor cardiac rhythm.

alex montana
October 17, 2025 AT 20:19Lidocaine IV infusion can knock down breakthrough pain in seconds!!!
Rohit Sridhar
October 19, 2025 AT 05:39When the opioid ceiling is hit, lidocaine steps in as a fast‑acting ally. Its rapid onset can bridge the gap while you titrate morphine down. Using the 1 mg/kg loading dose over ten minutes gives a noticeable dip in pain scores within half an hour. Keep the infusion below 2 mg/kg/h to stay in the safety zone, and you’ll often see less constipation and sedation. This approach empowers both patients and clinicians to reclaim quality of life in the final chapters.
kendra mukhia
October 20, 2025 AT 14:59Let’s be crystal clear: lidocaine isn’t a wonder‑drug, but it’s a powerhouse when used correctly. Its sodium‑channel blockade provides analgesia that opioids simply can’t mimic, especially for neuropathic components. The topical 4 % patch can soothe oral mucositis, while an IV infusion quenches visceral torment. Do not ignore the ceiling effect; exceeding 3 mg/kg/h invites seizures and arrhythmias. Monitoring serum levels after the first hour is non‑negotiable. And remember, every milligram saved on morphine translates to fewer opioid‑induced side effects. In short, lidocaine is the unsung sidekick that deserves a starring role in palliative protocols.
Bethany Torkelson
October 22, 2025 AT 00:19Don’t forget to monitor serum lidocaine levels whenever the infusion rate climbs above 2 mg/kg/h; early detection of toxicity saves lives.
Grace Hada
October 23, 2025 AT 09:39The ethical calculus of alleviating suffering mandates every tool be considered; lidocaine is a rational choice. Ignoring it is an affront to compassionate care.
Wyatt Schwindt
October 24, 2025 AT 18:59Lidocaine can be given topically, subcutaneously, or intravenously. Choose the route that matches the pain location. Keep dosing within recommended limits to avoid systemic toxicity.
Lyle Mills
October 26, 2025 AT 03:19From a pharmaco‑kinetic standpoint, lidocaine’s volume of distribution approximates 0.7 L/kg, facilitating rapid tissue penetration. When administered as a continuous IV infusion, the steady‑state concentration stabilizes within 30 minutes, allowing for titration against breakthrough pain indices. Electro‑physiological monitoring, particularly ECG for QRS widening, is essential once plasma levels approach 5 µg/mL. The adjunctive reduction in μ‑opioid equivalent dosing can mitigate opioid‑induced hyperalgesia, a phenomenon well documented in terminal oncology cohorts. In practice, integrating lidocaine into multimodal regimens enhances analgesic synergy without compounding opioid‑related adverse events.
Nhasala Joshi
October 27, 2025 AT 12:39The pharma giants don’t want you to know this 😱💊
Barbara Grzegorzewska
October 28, 2025 AT 21:59Honestly, the whole lidocaine discourse feels like a backstage pass to the elite pain‑management club. If you’re still stuck on oral morphine monotherapy, you’re basically playing checkers while the rest of us are on chess. The patch‑based delivery is sleek, discreet, and totally on‑point for mucosal lesions – think of it as the couture of analgesia. Stop slippin’ on outdated protocols and upgrade your palliative toolkit.
Nis Hansen
October 30, 2025 AT 07:19In the quiet moments of end‑of‑life care, the clinician’s greatest responsibility is to translate science into mercy. Lidocaine, a class‑Ib anti‑arrhythmic and local anesthetic, offers a pharmacologic bridge between rapid analgesia and a favorable side‑effect profile. By stabilizing neuronal membranes through reversible blockade of voltage‑gated sodium channels, it attenuates both somatic and neuropathic pain pathways. The pharmacodynamics are dose‑dependent, with low‑dose intravenous infusions producing analgesia without the profound central nervous system depression seen in opioids. A typical loading dose of 1 mg/kg over ten minutes establishes a therapeutic plasma concentration that often manifests as a pain score reduction of three to four points on the visual analog scale. Subsequent maintenance at 1–2 mg/kg/h can be sustained for 24‑48 hours, provided that vigilant monitoring for signs of toxicity is maintained. Early neurotoxic indicators-perioral tingling, metallic taste, or visual disturbances-should prompt an immediate assessment of serum lidocaine levels. Once concentrations exceed approximately 5 µg/mL, the risk of seizures escalates, necessitating rapid cessation of the infusion and administration of benzodiazepines if needed. Cardiovascular monitoring is equally critical, as high plasma levels may prolong the PR interval and widen the QRS complex, heralding potential arrhythmias. When used as an adjunct to high‑dose morphine, lidocaine can reduce overall opioid consumption by up to twenty percent, thereby alleviating constipation, sedation, and respiratory depression. Topical formulations, such as the 4 % lidocaine patch, provide targeted relief for mucosal ulcerations without systemic exposure, making them ideal for oral or dermal lesions. Peripheral nerve blocks with 0.5‑1 % lidocaine afford temporary but profound analgesia for localized cancer‑related neuropathy, especially when surgical interventions are no longer feasible. The interdisciplinary team must document dosing parameters, infusion rates, and observed effects in the patient’s chart to ensure continuity of care across shifts. Ethical considerations also arise: providing effective pain relief aligns with the principle of beneficence, while avoiding unnecessary drug interactions respects non‑maleficence. Ultimately, integrating lidocaine into a multimodal palliative regimen exemplifies a thoughtful, evidence‑based approach that honors the patient’s comfort and dignity in their final journey.
Fabian Märkl
October 31, 2025 AT 16:39Hey folks, great discussion on lidocaine! 🌟 It’s impressive how quickly an IV drip can turn a grim pain score into a manageable number. Just remember to keep the infusion rate in check and you’ll see fewer opioid side‑effects. Keep the conversation going! 🙌
Avril Harrison
November 2, 2025 AT 01:59Really insightful take – especially the bit about balancing beneficence and non‑maleficence in the bedside moment.