Desensitization Candidate Assessment Tool
This tool helps determine if you might be eligible for medication desensitization based on your reaction history and current medical needs. Remember, this is not a substitute for professional medical advice. Always consult with an allergist before proceeding.
Results
What if the only drug that can save your life is the one that nearly killed you before? For thousands of people each year, this isn’t a hypothetical question-it’s a real, urgent choice. Drug desensitization isn’t a miracle cure. It’s a carefully controlled medical process that lets someone who’s had a severe allergic reaction to a medication safely receive that same drug again. And it’s becoming more common than you think.
When Desensitization Is the Only Option
Desensitization isn’t used because it’s easy. It’s used because there’s no other way. When a patient has a life-threatening infection and only one antibiotic works, or when chemotherapy is the only treatment that shrinks their tumor, doctors don’t have room for alternatives. That’s when desensitization steps in.
According to research from Brigham and Women’s Hospital, this technique works in 95-100% of cases when done correctly. The key word here is correctly. It only works for certain types of reactions. If you’ve had hives, swelling, or trouble breathing within minutes of taking a drug like penicillin, carboplatin, or rituximab, you’re likely a good candidate. These are IgE-mediated reactions-the kind where your immune system overreacts fast and hard.
But if you got a severe rash weeks after taking a drug-like Stevens-Johnson syndrome or toxic epidermal necrolysis-desensitization is dangerous and not recommended. Those are T-cell-driven reactions, and trying to force your body to tolerate the drug can lead to fatal outcomes. Allergists don’t take this lightly. They review your history, test if needed, and only proceed if the benefits clearly outweigh the risks.
How Rapid Desensitization Works
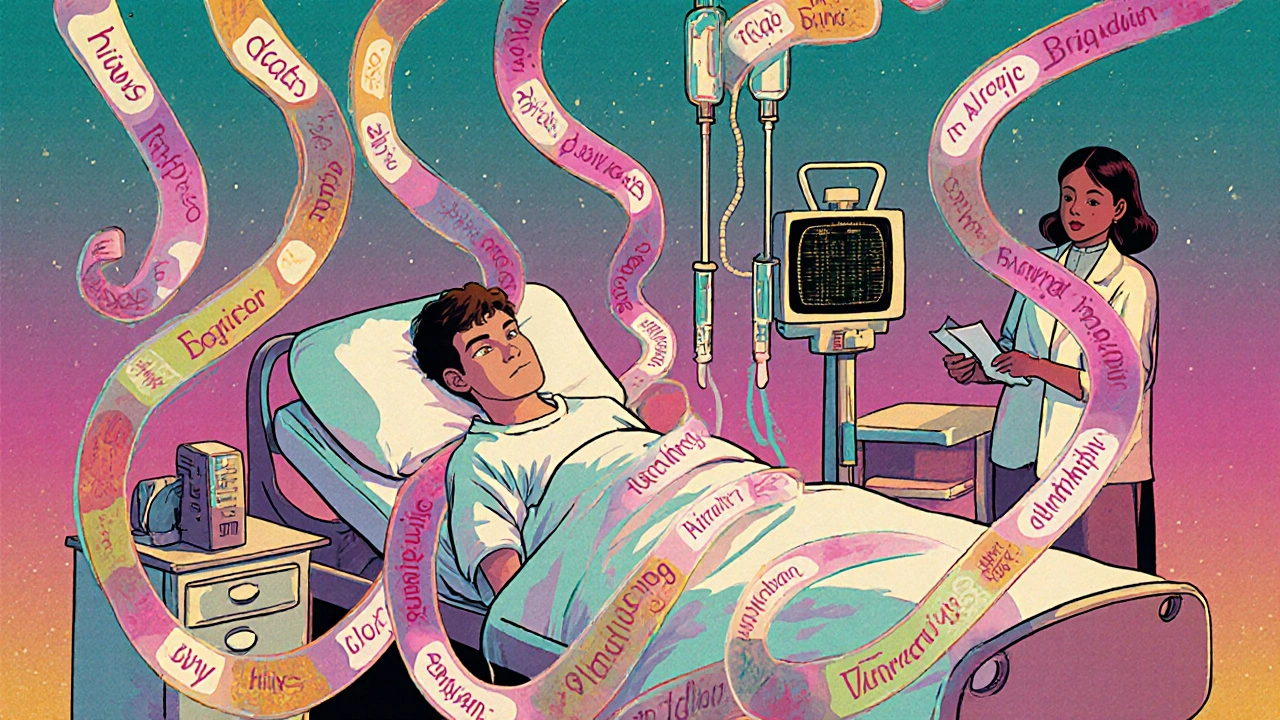
Rapid Drug Desensitization (RDD) is the most common method. It’s done in hospitals, under constant monitoring. The process starts with a tiny, almost undetectable dose-sometimes just one ten-thousandth of the full therapeutic amount. Then, every 15 minutes, the dose is doubled. After 12 steps, you’re at the full dose. The whole thing usually takes 4 to 6 hours.
It sounds intense, and it is. But here’s the science behind why it works: your immune cells get overwhelmed with small, repeated exposures. Instead of triggering a full-blown allergic response, they go quiet. It’s not a permanent fix. The tolerance lasts only as long as you keep taking the drug. Stop it for more than a day or two, and you’ll need to go through the whole process again.
For antibiotics like penicillin, this protocol has a 98% success rate. A 2022 study at Brigham and Women’s Hospital treated 42 patients with severe penicillin allergies. None had anaphylaxis. Only 8% had mild symptoms like flushing or itching. Every single patient finished their full course of antibiotics. That’s the kind of outcome that changes lives.
Slow Desensitization for Delayed Reactions
Not all reactions happen fast. Some take days-like the skin rashes or liver inflammation triggered by certain painkillers or antiretrovirals. For those, doctors use Slow Drug Desensitization (SDD). This isn’t as standardized as RDD. There’s no universal protocol. Some patients start with a tiny oral dose and increase it every 60 to 120 minutes. Others need days, not hours.
Aspirin desensitization, for example, often takes 2-3 days. Each dose is given hours apart, with careful monitoring for any sign of reaction. It’s slower, more tedious, but sometimes the only way to treat chronic sinusitis or asthma triggered by NSAIDs. Success rates are lower than RDD-around 70-80%-but still far better than avoiding the drug entirely.
Why Premedication Isn’t Enough
You might think, “Why not just give antihistamines or steroids before the drug?” That’s a common approach. But studies show it fails too often.
In one trial, 40 cancer patients got premedication before receiving taxane chemotherapy. Four of them still had severe reactions. That’s a 10% failure rate. Desensitization, in the same group, brought that down to less than 2%. Premedication masks symptoms-it doesn’t stop the immune system from reacting. Desensitization actually reprograms the response.
And here’s the kicker: many drugs have no safe alternatives. If you’re allergic to penicillin, you might be given vancomycin instead. But vancomycin is less effective for certain infections, more toxic to the kidneys, and contributes to antibiotic resistance. Desensitization lets you use the right drug, not just the safe one.
Who Shouldn’t Try It
Not everyone is a candidate. Desensitization is risky. It’s only for patients with no other options. Here’s when it’s a hard no:
- History of Stevens-Johnson syndrome or toxic epidermal necrolysis
- Severe delayed reactions with organ damage (liver, kidney, lungs)
- Uncontrolled asthma or unstable heart conditions
- Patients who’ve had prior fatal reactions
Even if you’ve had a mild rash before, doctors need to be sure it wasn’t a sign of something deeper. Misdiagnosing a reaction can be deadly. That’s why allergists are the only ones who should decide who qualifies.
The Hidden Costs and Challenges
Desensitization isn’t just about the protocol. It’s about resources. Each procedure takes 4.2 nursing hours and 1.8 physician hours. That’s a full workday for a team. Hospitals need trained staff, emergency equipment, and the right dilution kits.
Errors happen. In community hospitals, 8% of cases involve incorrect drug dilutions. In 15% of cases, patients are wrongly selected because staff don’t know the criteria. That’s why academic centers have success rates above 95%, while community hospitals see complications 40% more often.
Standardized checklists and simulation training have cut those errors dramatically. But not every hospital can afford it. That’s why desensitization is still rare outside major medical centers. In the U.S., only 35% of community hospitals offer it, even when it’s clearly needed.
What Patients Say
Patients who’ve gone through it often describe it as terrifying-but worth it.
One Reddit user, u/PenicillinWarrior, wrote: “After 20 years of being labeled allergic, the 4-hour protocol let me finally take the best antibiotic for my osteomyelitis.” Another, u/ChemoSurvivor, said: “My hospital didn’t have the proper dilution kits-took 3 attempts before they got it right.”
Surveys show 92% of oncology patients call it “life-saving.” But 63% admit to extreme anxiety during the process. That’s normal. You’re being given a drug that once made you sick. Your body is screaming danger. The medical team is there to calm it down-step by step.
The Future of Desensitization
This isn’t a static field. New research is making it smarter.
Scientists are now using biomarkers-like basophil activation tests-to predict who will respond before they even start. In a 2023 Lancet study, these tests predicted success with 89% accuracy. That means fewer failed attempts and less risk.
There are also early trials for home-based desensitization. For patients who’ve already completed the process once and are stable, doctors are testing whether they can safely take small, supervised doses at home. Early results show 92% success.
And in the next five years, experts like Dr. Mariana Castells believe genetic and immune profiling will determine not just if someone needs desensitization-but exactly which protocol will work best for them. Personalized medicine is coming to allergies.
The global market for desensitization is growing at 12.7% per year, mostly because cancer drugs and antibiotics are becoming more complex-and more likely to cause reactions. With antibiotic resistance killing 35,000 Americans each year, this isn’t just a medical procedure. It’s a public health tool.
Final Thoughts
Desensitization isn’t magic. It’s medicine at its most precise. It requires expertise, patience, and the right environment. But when used correctly, it turns a death sentence into a second chance.
If you’ve been told you can’t take a life-saving drug because of an allergy, ask: Have you seen an allergist? Have they evaluated whether desensitization is an option? Don’t accept “no” as the final answer. Sometimes, the only way forward is through the very thing that scared you most.
Can you desensitize to any drug?
No. Desensitization works best for immediate, IgE-mediated reactions-like hives, swelling, or anaphylaxis that happen within minutes of taking a drug. It’s commonly used for antibiotics (penicillin), chemotherapy drugs (taxanes, platinum agents), and monoclonal antibodies. It does not work for severe delayed reactions like Stevens-Johnson syndrome, toxic epidermal necrolysis, or organ damage that occurs days later. Those reactions involve different immune pathways and are too dangerous to attempt.
How long does the desensitization effect last?
The tolerance is temporary. If you stop taking the drug for more than 48 hours, your immune system can “remember” the allergy. That means you’ll need to go through the full desensitization process again before your next dose. This is why it’s only used for medications you need to take repeatedly-like daily antibiotics or weekly chemotherapy. It’s not for one-time use.
Is desensitization safe?
When performed by trained allergists in a fully equipped facility, it’s very safe. Severe reactions occur in less than 2% of cases. Most side effects are mild-flushing, itching, or low-grade fever. But if done incorrectly-in a clinic without emergency equipment or by staff who haven’t been trained-it becomes dangerous. Studies show complication rates triple in non-specialized settings. That’s why it should only be done in hospitals or allergy centers with anaphylaxis protocols ready.
Can I do this at home?
Not for the first time. The initial desensitization must be done under close medical supervision. But for patients who’ve successfully completed the process and are stable, early trials are testing home-based protocols for maintenance doses. These are still experimental and only offered in research settings. If you’re considering this, ask your allergist about ongoing clinical trials.
What if I’m allergic to penicillin but need an antibiotic?
Many people are misdiagnosed with penicillin allergy. Up to 90% of those who report it aren’t truly allergic after proper testing. If you’ve never been evaluated by an allergist, start there. Skin testing can confirm if you’re still allergic. If you are, rapid desensitization is highly effective-98% success rate-and lets you take the best antibiotic for your infection. Avoiding penicillin often means using broader-spectrum drugs that increase resistance and side effects.
How do I find a doctor who does this?
Look for an allergist-immunologist affiliated with a major hospital or academic medical center. Community clinics rarely offer this service. You can search through the American Academy of Allergy, Asthma & Immunology (AAAAI) directory or ask your oncologist or infectious disease specialist for a referral. Be prepared to travel-many centers require appointments weeks in advance because of the time and resources needed.
Dana Dolan
November 19, 2025 AT 12:10i literally cried reading this. after my mom went through penicillin desensitization for her osteomyelitis, i thought i’d never see her walk again without that IV. but she did. 4 hours, 12 steps, and she’s been fine for 3 years now. thank you for writing this. 🥹
Michael Petesch
November 19, 2025 AT 17:40This is an exceptionally well-researched and clearly articulated overview of a critically underutilized clinical protocol. The distinction between IgE-mediated and T-cell-mediated reactions is particularly vital, as misclassification can lead to catastrophic outcomes. I would encourage healthcare institutions to implement mandatory allergist consultation pathways for patients with reported drug allergies prior to alternative antibiotic selection.
Richard Risemberg
November 19, 2025 AT 20:06Yo, this isn’t just medicine-it’s a goddamn miracle on a drip line. 🤯 Imagine being told you can’t take the one thing that’ll save you… then finding out you can, if you’re brave enough to let them slowly, carefully, *baby-step* you back into life. I’ve seen chemo patients turn from ghosts to grinning idiots after desensitization. It’s not magic. It’s science with heart. And yeah, it’s expensive. But so is burying someone who could’ve lived. Let’s fund this stuff.
Andrew Montandon
November 20, 2025 AT 09:14Wait-so if you stop the drug for more than 48 hours, you have to do the whole thing over again? That’s insane! And why aren’t we doing this for EVERYONE who’s allergic? I mean, 90% of people who say they’re allergic to penicillin aren’t even allergic? That’s wild. And why do community hospitals mess up dilutions 8% of the time? That’s not incompetence-that’s negligence. We need mandatory certification for staff who touch these protocols. Like, now. 🚨
Sam Reicks
November 21, 2025 AT 05:57theyre lying about desensitization its a government mind control experiment to make you take more drugs and get addicted to them. the immune system knows what its doing. why would you force it to accept poison? the real cure is herbal remedies and avoiding all pharmaceuticals. also the 95% success rate? fabricated by big pharma. they make money off repeat procedures. dont trust hospitals. trust nature.
Chuck Coffer
November 22, 2025 AT 20:13So let me get this straight. You’re telling me we’ve spent decades telling people to avoid penicillin… and now we’re just going to *force* their bodies to accept it? How is that different from psychological abuse? And why are we not asking why the drug causes these reactions in the first place? Maybe the drug is the problem, not the person. Just saying.
Derron Vanderpoel
November 24, 2025 AT 08:10my brother went through this for carboplatin. he was terrified. like, sobbing in the chair before they started. but the nurses held his hand, talked him through every step, and when he got to the full dose? he laughed. said it felt like winning a marathon. he’s been in remission for 2 years now. i still get emotional thinking about it. thank you for sharing this. people need to know this is real. it’s not just a procedure-it’s hope.
Timothy Reed
November 26, 2025 AT 06:48Thank you for providing such a comprehensive and clinically accurate summary. The emphasis on distinguishing between reaction types is essential for patient safety. I would add that standardized institutional protocols and interdisciplinary training are key to reducing error rates in community settings. Collaboration between oncology, infectious disease, and allergy departments is not optional-it is imperative.
Christopher Robinson
November 26, 2025 AT 10:5798% success rate with penicillin? 🤯 that’s wild. i’ve got a friend who’s been avoiding all antibiotics for 15 years because of a rash she got as a kid. she just found out she’s not even allergic. she’s gonna cry. seriously. if you think you’re allergic to something, get tested. don’t live in fear. this is the kind of info that changes lives. 🙌❤️