Chlorambucil isn’t a drug you hear about every day. But if you or someone you love is facing chronic lymphocytic leukemia (CLL) or certain types of non-Hodgkin lymphoma, it might be one of the first treatments your doctor suggests. It’s old. It’s cheap. And for many people, it’s the only option that makes sense-financially and medically. But here’s the real question: chlorambucil cost might look low on paper, but is it really worth it?
What Is Chlorambucil, Really?
Chlorambucil is a chemotherapy drug that’s been around since the 1950s. It belongs to a group called alkylating agents. These drugs work by damaging the DNA inside cancer cells so they can’t multiply. Unlike newer targeted therapies or immunotherapies, chlorambucil doesn’t pick and choose. It hits fast-dividing cells-cancerous or not. That’s why side effects like low blood counts, nausea, and fatigue are common.
It’s not used for aggressive cancers. It’s for slower-moving ones-like early-stage CLL in older adults, or patients who can’t tolerate stronger treatments. In New Zealand, Australia, and parts of Europe, it’s still a first-line option because it works well enough, and it’s easy to take as a pill at home. No IVs. No hospital visits. Just a daily tablet.
How Much Does Chlorambucil Actually Cost?
In the United States, a 30-day supply of chlorambucil can cost anywhere from $150 to $400 without insurance. That sounds high-until you compare it to newer drugs. Ibrutinib? $15,000 a month. Venetoclax? $12,000. Even bendamustine, another chemo, runs $5,000-$8,000 per cycle.
In countries with public healthcare-like New Zealand, the UK, or Canada-chlorambucil is often free or nearly free for patients. The government buys it in bulk, and the price per tablet is under $1. In New Zealand, Pharmac covers it fully under the public drug schedule. You pay nothing at the pharmacy if you have a prescription.
But here’s the catch: if you’re in the U.S. and uninsured, or if your insurance has a high deductible, that $400 a month adds up fast. Over six months? That’s $2,400. A year? Nearly $5,000. For someone on a fixed income, that’s a real burden. And that’s just the drug. You still need blood tests every few weeks. Doctor visits. Maybe a hospital stay if your counts drop too low.
What’s the Real Cost Beyond the Price Tag?
Money isn’t the only cost. Time is. Fatigue is. Risk is.
Chlorambucil works slowly. It might take three to six months before you see results. During that time, you’re still living with symptoms-swollen lymph nodes, night sweats, feeling worn out. You’re not getting better fast. You’re just not getting worse as quickly.
Side effects are real. Low white blood cells mean you’re more likely to get infections. Low platelets mean you bruise easily or bleed for longer. Some people develop anemia and need transfusions. In rare cases, chlorambucil can lead to secondary cancers years later, like leukemia. That’s why doctors don’t use it for young, healthy patients.
And then there’s the emotional toll. Taking a drug that’s 70 years old can feel like settling. Like you’re not getting the ‘best’ treatment. But the truth? For many older adults, especially those over 70 with other health issues, chlorambucil is the safest option. Newer drugs have their own risks-heart problems, bleeding, severe diarrhea. Chlorambucil’s risks are predictable. You know what you’re getting.

Who Benefits Most From Chlorambucil?
It’s not for everyone. But for specific groups, it’s a lifeline:
- Patients over 70 with early-stage CLL and no high-risk genetic markers
- People with kidney problems who can’t handle stronger chemo
- Those who can’t afford or access newer therapies
- Patients who prefer oral treatment over IV infusions
- People in countries without universal drug coverage but with access to generic chlorambucil
In the U.S., the National Comprehensive Cancer Network (NCCN) still lists chlorambucil as an option for older CLL patients. The American Society of Hematology doesn’t push it aside-it just says, ‘Use it wisely.’
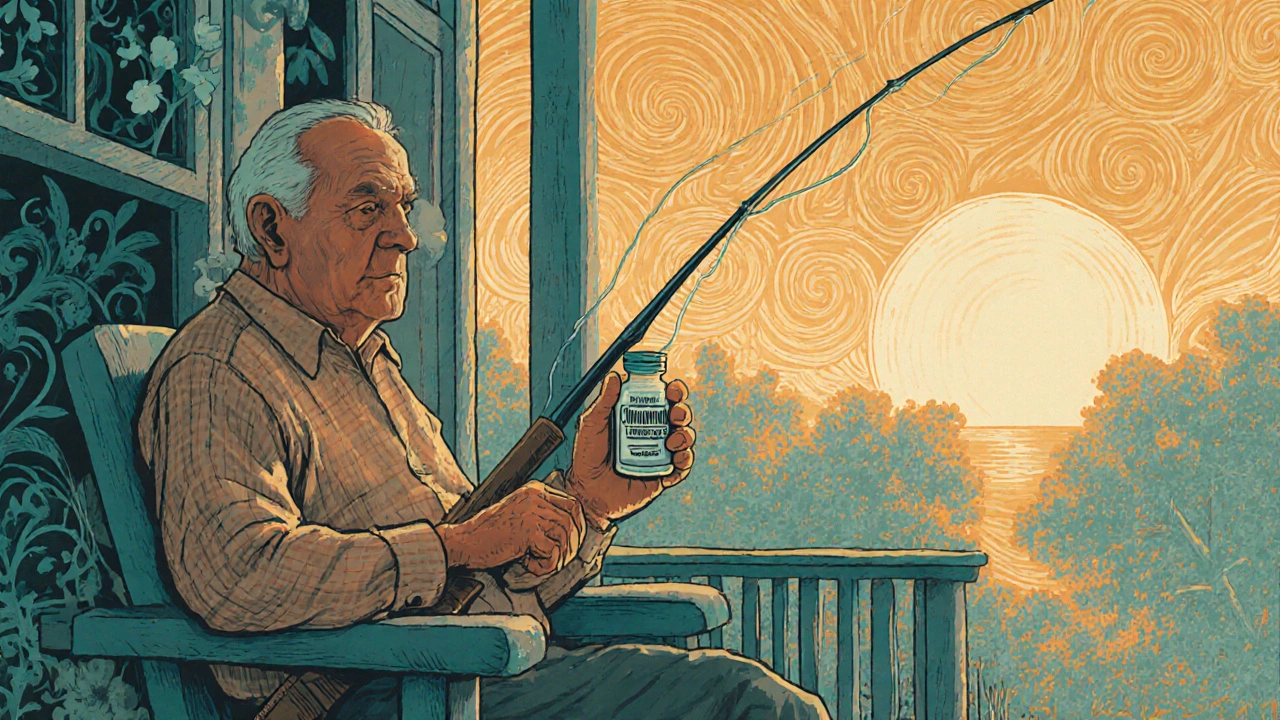
One 74-year-old man in Wisconsin told his oncologist he couldn’t afford the $18,000-a-month drug he was offered. His doctor switched him to chlorambucil. He’s been on it for three years. His cancer is stable. He’s still fishing on weekends. He didn’t get a miracle. But he got time. And he didn’t go bankrupt.
Chlorambucil vs. Newer Drugs: A Quick Comparison
| Feature | Chlorambucil | Ibrutinib | Venetoclax | Fludarabine + Cyclophosphamide |
|---|---|---|---|---|
| Cost (U.S., monthly) | $150-$400 | $14,000-$16,000 | $11,000-$13,000 | $5,000-$8,000 |
| Form | Oral pill | Oral pill | Oral pill | IV infusion |
| Time to effect | 3-6 months | 1-3 months | 2-4 months | 1-2 months |
| Common side effects | Low blood counts, nausea, fatigue | Diarrhea, bruising, high blood pressure | Low neutrophils, tumor lysis syndrome | Severe immune suppression, infections |
| Long-term cancer risk | Yes, rare | Low | Low | Yes, higher than chlorambucil |
| Best for | Older, frail patients, low budget | Patients needing fast response, no kidney issues | Patients with high-risk genetics | Younger, fit patients |
Chlorambucil doesn’t win on speed. It doesn’t win on fancy science. But it wins on accessibility. On simplicity. On being there when nothing else is.

Is It Worth It? The Answer Depends on You
There’s no one-size-fits-all answer. For a 68-year-old woman in rural New Mexico with Medicare and a $5,000 deductible, chlorambucil might be the only choice that lets her keep her home. For a 55-year-old in London with full NHS coverage, it’s just another tool in the box.
What makes chlorambucil worth it? Three things:
- You need a treatment that’s affordable and doesn’t require constant medical oversight
- You’re not looking for a cure-you’re looking for control
- You value quality of life over aggressive intervention
If you’re young, fit, and have high-risk cancer? It’s probably not the right choice. But if you’re older, managing other health issues, or just trying to avoid financial ruin? It might be the smartest thing you do.
Doctors don’t push chlorambucil because it’s outdated. They use it because it still works-and because for many people, nothing else does.
Frequently Asked Questions
Is chlorambucil still used today?
Yes. While newer drugs are more common in wealthy countries, chlorambucil is still a standard treatment for older adults with chronic lymphocytic leukemia, especially in places where cost matters. Guidelines from the NCCN and European Society for Medical Oncology still include it as an option.
Can I get chlorambucil without insurance?
In the U.S., it’s possible. Generic chlorambucil is one of the cheapest chemotherapy drugs available. Some pharmacies offer it for under $100 a month through discount programs. Nonprofits like the Patient Access Network Foundation may help cover costs. Always ask your pharmacist or oncologist about patient assistance programs.
Does chlorambucil cause hair loss?
Not usually. Unlike many chemo drugs, chlorambucil rarely causes complete hair loss. Some people notice thinning, but most keep their hair. That’s one reason it’s preferred for patients who want to maintain a sense of normalcy during treatment.
How long do people stay on chlorambucil?
It’s often taken for months or even years. Treatment usually starts with daily doses for 4-6 weeks, then moves to every other day or weekly. Doctors monitor blood counts closely. If the cancer responds and side effects stay manageable, treatment can continue long-term. Some patients stay on it for over five years.
Are there alternatives to chlorambucil if I can’t afford it?
Yes. In the U.S., bendamustine is a common alternative, though it’s more expensive. Outside the U.S., in countries with public health systems, chlorambucil is usually the default because it’s the most cost-effective. If cost is the barrier, talk to your doctor about clinical trials or drug assistance programs-many offer free or low-cost access to newer therapies for qualifying patients.
What Comes Next?
If you’re considering chlorambucil, don’t make the decision alone. Ask for a second opinion. Ask about financial aid. Ask what happens if it stops working. Ask how you’ll know if it’s helping.
Chlorambucil isn’t glamorous. But for thousands of people around the world, it’s the difference between staying at home and being stuck in a hospital. Between paying the mortgage and filing for bankruptcy. Between watching your grandkids grow up and not being there at all.
It’s not about choosing the newest drug. It’s about choosing the right one-for your body, your life, and your future.
Dana Dolan
November 20, 2025 AT 03:06Wow, this post really hit home. My dad was on chlorambucil for 4 years after his CLL diagnosis. He never lost his hair, kept fishing every weekend, and never went broke. People act like it’s ‘old school’ like it’s a bad thing - but sometimes old school is the only thing that keeps you alive without losing your house.
Nick Lesieur
November 20, 2025 AT 17:31lol so the ‘solution’ is just give people chemo from the 50s? 🤡 Next they’ll bring back leeches and bloodletting. This is what happens when you let capitalism kill innovation. Also, who still takes pills for cancer? I’m getting my IV drip with a margarita.
Angela Gutschwager
November 21, 2025 AT 20:13Chlorambucil is cheap but it’s not magic. My aunt got it and ended up in the ER 3x from infections. Still cheaper than $15k/month tho. 😅
Andy Feltus
November 21, 2025 AT 23:41It’s funny how we treat medicine like a tech product - newer always means better. But chlorambucil isn’t a buggy app. It’s a tool. A blunt, slow, cheap tool that still cuts through the noise. We don’t need a Tesla when a bicycle gets you to the same place without bankrupting you. The real tragedy isn’t the drug - it’s that we’ve made access to basic care a luxury.
Dion Hetemi
November 22, 2025 AT 14:57Let’s be real - this is just the pharma industry’s way of keeping the poor alive long enough to pay for their blood tests and ER visits. Chlorambucil isn’t ‘worth it’ - it’s what’s left after the system stripped everything else away. And don’t even get me started on how they market this as ‘smart’ instead of ‘desperate.’
Kara Binning
November 24, 2025 AT 14:26So now we’re glorifying 70-year-old poison because Americans can’t afford healthcare? This is why the U.S. is a joke. In Canada, we get the latest drugs for free - no ‘settlement’ required. If you’re okay with dying slowly because you’re too poor to get real treatment, that’s your choice. But don’t call it wisdom - call it failure.
Zac Gray
November 26, 2025 AT 06:28Look, I get the outrage. I really do. But let’s not pretend this is about ‘choice.’ For a lot of people - especially older folks with Medicare Part D gaps, no supplemental insurance, and a fixed income - chlorambucil isn’t a preference. It’s the only door left open. I’ve seen too many patients cry because they had to choose between chemo and insulin. This isn’t about being ‘old school.’ It’s about a system that forces people to pick between their life and their home. And yeah, maybe it’s not glamorous. But dignity isn’t always found in a shiny new pill. Sometimes it’s just in being able to sit on your porch and watch the sunset without wondering how you’ll pay for tomorrow’s dose.
Steve and Charlie Maidment
November 26, 2025 AT 07:13Interesting how the article casually mentions ‘in New Zealand it’s free’ like that’s normal. Meanwhile, here in the U.S., we’re supposed to be impressed that someone’s paying $400 a month? That’s still a fortune to a lot of people. And don’t even get me started on how the table compares costs without mentioning that newer drugs often come with side effects that require additional meds, hospital stays, and specialist visits - which all add up. Chlorambucil’s ‘low cost’ is only low if you ignore the hidden costs of managing its side effects. And yet, nobody talks about that. Because the system doesn’t want you to see the full picture.
Michael Petesch
November 26, 2025 AT 11:44As someone who’s studied global health policy for over a decade, this post encapsulates a critical but under-discussed truth: access to care is not a function of medical efficacy, but of economic structure. Chlorambucil’s continued use is not a testament to its superiority, but to the failure of market-driven healthcare systems to deliver equitable access. In nations with universal pharmacare, it is used not out of necessity, but because it is a safe, effective, and appropriately indicated option - no stigma attached. In the U.S., it’s a symbol of systemic abandonment. The real question isn’t whether chlorambucil is worth it - it’s why we’ve allowed a 70-year-old drug to become a proxy for justice.