Imagine skipping 36 human clinical trials to prove a generic drug works the same as the brand-name version. Sounds too good to be true? It’s not. That’s the power of IVIVC-In Vitro-In Vivo Correlation. It’s a scientific bridge between a drug’s behavior in a lab dish and how it actually performs inside the human body. And for complex generic medicines, it’s becoming the smarter, faster, cheaper way to get to market.
What IVIVC Really Means (And Why It Matters)
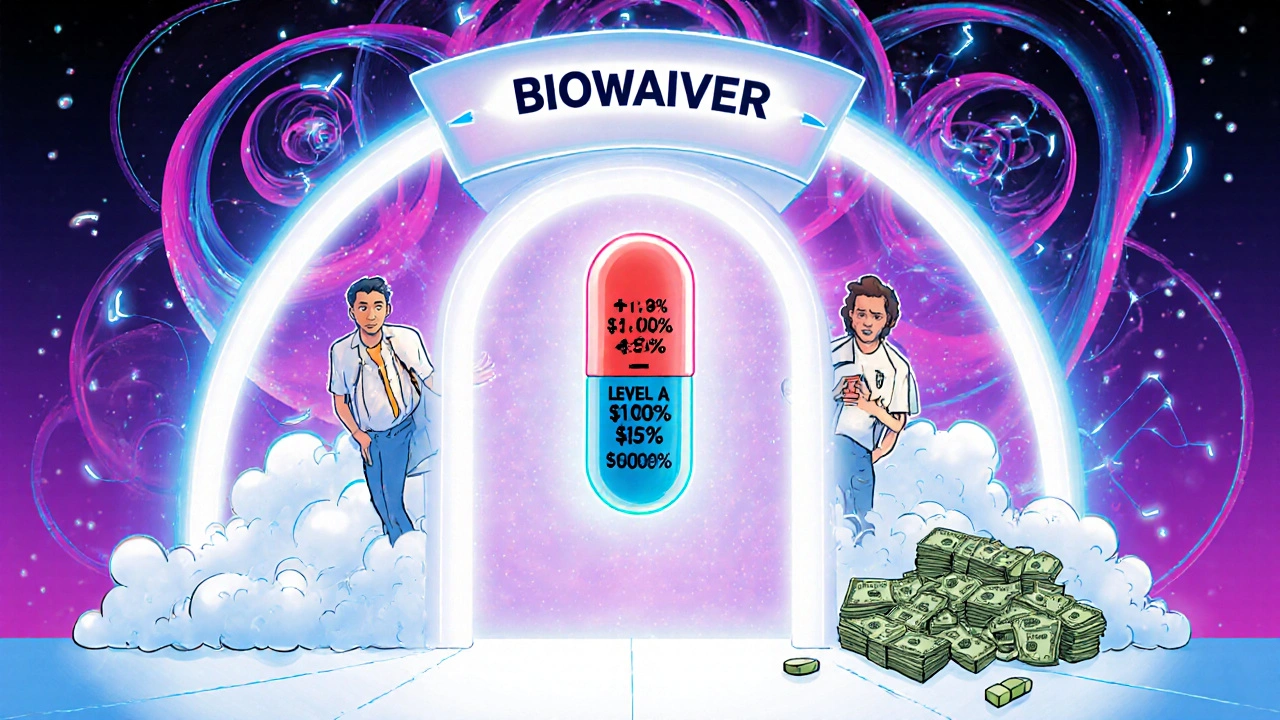
IVIVC isn’t just fancy jargon. It’s a mathematical model that links how fast a drug dissolves in a test tube (in vitro) to how quickly it gets absorbed into the bloodstream (in vivo). If you can reliably predict what happens in the body just by watching a tablet dissolve in a machine, you don’t need to give it to healthy volunteers. That’s a biowaiver-official permission to skip the human study.
The U.S. FDA first laid out the rules in 1996. Since then, the framework has been refined, especially in the 2014 guidance. The European Medicines Agency (EMA) follows similar standards. The goal? Reduce waste. A single bioequivalence study costs between $500,000 and $2 million. It takes months to recruit volunteers, run tests, and analyze results. IVIVC cuts that down to weeks and saves millions per product.
But here’s the catch: IVIVC doesn’t work for every drug. It’s most powerful for modified-release tablets-those that slowly release medicine over 8, 12, or even 24 hours. For simple immediate-release pills, the Biopharmaceutics Classification System (BCS) often does the job. But when the release mechanism is complex-think patches, capsules with beads, or extended-release pellets-IVIVC is often the only viable path to a waiver.
The Four Levels of IVIVC: Which One Actually Works?
Not all correlations are created equal. The FDA defines four levels, and only one truly lets you skip human trials without heavy backup.
- Level A: The gold standard. It matches dissolution at every single time point to blood concentration at the exact same time. Think of it like a perfect mirror. If the drug dissolves 40% at 1 hour in the lab, it should hit 40% absorption in the body too. This requires an R² value over 0.95 and a slope close to 1.0. Only Level A is accepted for full biowaivers.
- Level B: Uses averages-mean dissolution time vs. mean residence time. Less precise. Not enough for a waiver on its own.
- Level C: Links one dissolution number (like % dissolved at 1 hour) to one PK number (like Cmax). It’s easier to build but risky. The EMA and FDA warn it can miss real-world variations, especially with food effects or patient differences.
- Multilevel C: Several Level C points combined. Sometimes accepted if backed by strong data, but still not as reliable as Level A.
For regulators, the bar is strict: any IVIVC model must predict AUC within ±10% and Cmax within ±15%. If it’s off by more, the waiver gets rejected.
Why Most IVIVC Submissions Fail
According to FDA data from 2023, 64% of IVIVC submissions were turned down-not because the science was bad, but because the setup was flawed. Here’s what goes wrong most often:
- Non-physiological dissolution conditions: Testing a drug in plain water at pH 6.8 doesn’t reflect the stomach’s acidic environment or the bile salts in the small intestine. Biorelevant media-those that mimic real gut fluid-have become essential. Companies still skip this to save time. Big mistake.
- Too few formulations: To build a good model, you need at least 3-5 versions of the drug with different release rates. Some companies try to skip this and test only one or two. The model then can’t capture how changes affect absorption.
- Poor PK data: You need dense blood sampling-12+ time points per volunteer. If you only take samples at 1, 2, 4, and 8 hours, you’re missing the curve. The FDA sees this all the time.
- Weak validation: You can’t just fit a curve to your data. You have to test it on a new set of formulations you didn’t use to build the model. Most failed submissions skip this step.
A 2022 survey of 47 generic drug companies found that 76% of IVIVC failures were due to insufficient formulation characterization. In other words, they didn’t make enough different versions of the drug to truly understand how it behaves.
Who’s Doing It Right?
Some companies get it. Teva spent 14 months and three formulation tries to build a Level A IVIVC for an extended-release oxycodone generic. The payoff? They avoided five full bioequivalence studies. That’s over $10 million saved.
Contract labs like Alturas Analytics and Pion report success rates of 60-70% when they’re brought in early. Why? They know the pitfalls. They use biorelevant media. They design the dissolution method to detect even 10% changes in polymer content. They collect PK data with 16-20 time points. They validate on unseen batches.
Meanwhile, smaller companies often try to do it in-house and fail. Only about 15% of pharma firms have the in-house expertise. The rest either partner with CROs or give up.
When IVIVC Won’t Work (And What to Do Instead)
IVIVC is not magic. It fails when:
- The drug has a narrow therapeutic index-like warfarin or digoxin. Even small absorption differences can be dangerous.
- The absorption is nonlinear-meaning doubling the dose doesn’t double the blood level.
- The drug’s absorption depends heavily on food, pH, or gut motility. IVIVC models can’t fully replicate those variables.
- You’re dealing with injectables, ophthalmics, or inhalers. These are harder to correlate, and regulators are still building the rules.
For those cases, you still need human studies. But even here, IVIVC can help. It can guide formulation changes to minimize the number of studies needed. For example, if you know your dissolution profile shifts slightly after a manufacturing change, you can predict whether a full BE study is needed-or if a simple dissolution comparison is enough.
The Future: Biorelevant Media, AI, and Global Harmonization
By 2025, 75% of new IVIVC submissions are expected to use biorelevant dissolution media, according to the American Association of Pharmaceutical Scientists. That’s a big shift from the old standard of testing in plain buffer solutions.
Machine learning is also creeping in. Both the FDA and EMA are open to AI-driven models-if they’re transparent and scientifically sound. Imagine training an algorithm on thousands of past dissolution and PK datasets to predict correlation without manual curve-fitting. It’s happening.
Regulators are also expanding the scope. In June 2023, the FDA released draft guidance for IVIVC in topical products. The EMA’s 2021 reflection paper showed that 23% of scientific advice requests now involve IVIVC. And with GDUFA III funding $15 million for IVIVC research through 2027, this isn’t a trend-it’s a transformation.
By 2027, IVIVC-supported biowaivers could account for 35-40% of all modified-release generic approvals, up from 22% in 2022. The companies that invest in this now will dominate the next decade of generic drug development.
How to Get Started (If You’re Building a Generic)
If you’re developing a complex generic and want to use IVIVC:
- Start early-during prototype development, not right before filing.
- Design 3-5 formulations with different release rates (vary polymers, fillers, coating thickness).
- Use biorelevant dissolution media (fasted and fed state simulations).
- Run pharmacokinetic studies with 12-24 subjects per formulation, sampling every 15-30 minutes for the first 8 hours.
- Work with a CRO experienced in IVIVC. Don’t try to build the model alone.
- Validate the model on formulations you didn’t use to build it.
- Document everything. Regulators will ask for every detail.
It’s not easy. But for the right product, it’s the only way to compete on cost, speed, and scale.
What is IVIVC and how does it relate to bioequivalence?
IVIVC stands for In Vitro-In Vivo Correlation. It’s a scientific model that links how a drug dissolves in a lab test (in vitro) to how it’s absorbed in the human body (in vivo). When this correlation is strong and validated, regulators like the FDA and EMA can allow a biowaiver-meaning you don’t need to run expensive human bioequivalence studies to prove your generic drug works the same as the brand.
Can IVIVC be used for all types of drugs?
No. IVIVC works best for modified-release oral products like extended-release tablets or capsules. It’s not reliable for drugs with narrow therapeutic indexes (like warfarin), nonlinear absorption, or those affected strongly by food. It’s also still experimental for injectables, eye drops, and inhalers. For simple immediate-release drugs, the Biopharmaceutics Classification System (BCS) is often used instead.
What’s the difference between Level A and Level C IVIVC?
Level A is a point-to-point correlation-every dissolution time point matches a blood concentration time point exactly. It’s the only level accepted for full biowaivers. Level C links just one dissolution value (like % dissolved at 1 hour) to one pharmacokinetic value (like Cmax). It’s easier to create but doesn’t predict the full absorption profile and is riskier for regulators to accept.
Why do most IVIVC submissions get rejected?
The top reasons are: using non-physiological dissolution media (like plain water instead of simulated gut fluid), testing too few formulations (less than 3), not collecting enough blood samples (fewer than 12 time points), and failing to validate the model on new batches. The FDA found 64% of rejections in 2023 were due to poor physiological relevance.
How much does it cost to develop an IVIVC model?
Developing a Level A IVIVC typically costs $1-2 million and takes 12-18 months. This includes formulation development, dissolution testing, pharmacokinetic studies, and modeling. But it saves $500,000-$2 million per bioequivalence study you avoid. For complex products with multiple post-approval changes, the long-term savings can exceed $10 million.
Is IVIVC accepted globally?
Yes. Both the U.S. FDA and the European EMA accept IVIVC for biowaivers, especially for oral extended-release products. Approval rates have risen from 15% in 2018 to 42% in 2022 as companies improve their methods. Other regions like Japan and Canada follow similar standards, though acceptance for non-oral products is still evolving.

doug schlenker
November 27, 2025 AT 18:56Man, I've seen so many startups try to cut corners with IVIVC and then get slapped by the FDA. It's not magic-it's hard science. But when it works? It's like having a cheat code for generic drug approval. Saved my company millions last year on an extended-release patch project.
Just make sure you use biorelevant media. Plain water at pH 6.8 is a joke. Your drug doesn't live in a lab beaker-it lives in a gut full of bile and enzymes.
Olivia Gracelynn Starsmith
November 28, 2025 AT 04:39IVIVC is the future but most people don't realize how much work goes into it. You can't just run one dissolution test and call it a day. You need at least three formulations with different release profiles and dense PK sampling. And validation? Non-negotiable. If you skip that, you're just wasting everyone's time.
Also don't forget the food effect. If your drug behaves differently after a high-fat meal, your model better account for it. Otherwise you're setting yourself up for failure.
Skye Hamilton
November 29, 2025 AT 10:48So you're telling me we're trusting a machine that dissolves pills in fake stomach juice to predict how humans will react to drugs? Cool. So next they'll just scan my DNA and say I'm healthy. No need for doctors or blood tests right? Just let the algorithm decide.
Also who funded this post? Big Pharma? Because this sounds like a slick ad for skipping safety checks. I've seen what happens when we let algorithms replace human trials. Remember Vioxx? Yeah. Thought so.
Maria Romina Aguilar
November 30, 2025 AT 16:56Level A IVIVC... is the only acceptable model... for biowaivers... according to the FDA... 1996 guidance... and reaffirmed... in 2014... and even then... only if... R² > 0.95... and slope... is within... 0.95–1.05... and AUC... within ±10%... and Cmax... within ±15%... and dissolution... must be... in biorelevant media... and PK sampling... must be... every 15–30 minutes... for 8 hours... and validation... must be... on unseen batches... and formulation... must include... at least three... variants... and you must... document... every single... parameter... or else... rejection... guaranteed... and... you... will... cry... in your... office... at 3am... again...
Brandon Trevino
December 1, 2025 AT 05:4764% rejection rate? That's not failure. That's incompetence. You don't get to skip human trials unless your model is bulletproof. Most submissions fail because they treat IVIVC like a PowerPoint slide deck instead of a rigorous statistical framework. You need multivariate regression, cross-validation, and physiologically based modeling-not a linear fit in Excel.
And don't even get me started on companies using non-biorelevant media. That's not science. That's corporate negligence dressed up as innovation.
Denise Wiley
December 1, 2025 AT 08:15OMG I just read this and I'm so excited!! This is the kind of stuff that makes generics affordable!! I work with patients who can't afford brand-name meds and knowing that we can get safe, effective generics faster? That's a win for real people.
Also shoutout to Teva for doing it right-14 months of work? Worth it. They didn't cut corners. They did the hard thing. And now people get their meds cheaper. That's the dream right there.
Hannah Magera
December 1, 2025 AT 17:19So if I'm making a generic pill that releases over 12 hours, I need to make 3-5 versions with different coatings or polymers? And then test them all in something that looks like actual stomach fluid? And take blood every 30 minutes for 8 hours?
That sounds like a lot. But if it saves me from doing 5 human studies, then yeah, it's worth it. I think I get it now. Thanks for explaining it so clearly.
Austin Simko
December 3, 2025 AT 06:57They're not replacing human trials. They're hiding them. The data is still collected. It's just buried in corporate labs. And who's watching? The FDA? Ha. They're understaffed and underfunded. This is just corporate greed with a sciencey name.
Nicola Mari
December 4, 2025 AT 17:15How utterly reckless. To replace human testing with laboratory simulations? This is the logical endpoint of deregulation and profit-driven medicine. You think a machine can replicate the complexity of the human gastrointestinal tract? You are deluding yourselves. This is not progress. It is hubris.
And yet, somehow, the same people who champion this will scream about 'natural remedies' and 'biohacking' when it suits them. Hypocrites all.
Sam txf
December 5, 2025 AT 21:06Level A IVIVC is the only thing that matters. Everything else is just noise. If you're not hitting R² > 0.95 and slope = 1.0, you're not even in the game. And if you're using plain buffer? You're not even trying. The FDA doesn't care how much you spent. They care if your model predicts real human absorption. Period.
Also, AI models are coming. They're already training on 10,000+ historical datasets. In 2 years, you'll either adapt or get left behind. No one's gonna wait for your outdated methods.