Opioid Dosing Calculator for Liver Disease
Opioid Dosing Calculator
Dosing Guidance
This calculator adjusts dosing based on liver disease severity to minimize overdose risk. All recommendations align with medical guidelines for impaired liver function.
Important Note: Always consult with a healthcare provider before adjusting any medication. This tool provides general guidance only.
When someone has liver disease, taking opioids isn't just about managing pain-it’s a balancing act with serious risks. The liver doesn’t just filter toxins; it breaks down most opioids. When it’s damaged, that process slows down or stops, and drugs build up in the body. What’s meant to be a safe dose can turn into an overdose. This isn’t theoretical. People with cirrhosis or advanced fatty liver disease are far more likely to experience dangerous side effects from opioids-even at normal prescribed doses.
How the Liver Normally Processes Opioids
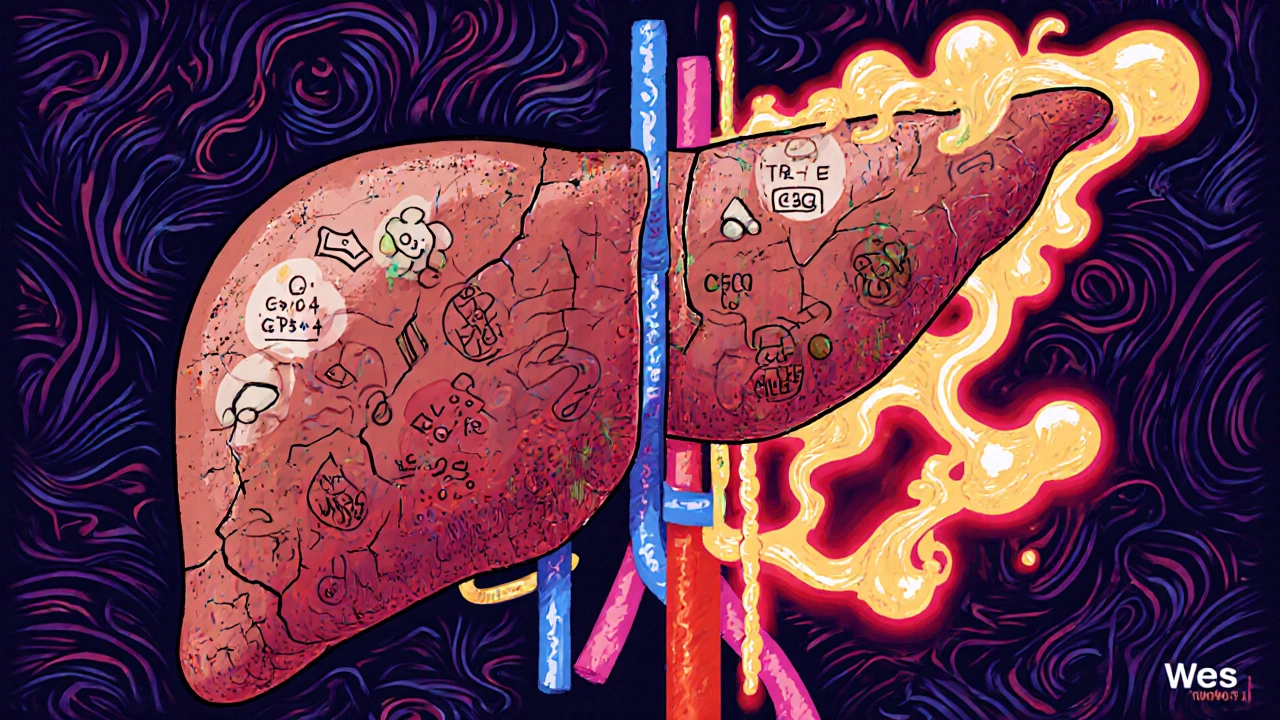
The liver uses two main systems to break down opioids: cytochrome P450 enzymes and glucuronidation. These are like specialized factories inside liver cells. CYP3A4 and CYP2D6 are the two most important enzymes for opioids like oxycodone and hydrocodone. Morphine, on the other hand, doesn’t rely on CYP enzymes-it gets turned into two different metabolites through glucuronidation: morphine-6-glucuronide (M6G), which helps with pain relief, and morphine-3-glucuronide (M3G), which can cause seizures and confusion.
In a healthy liver, these metabolites are cleared quickly through the kidneys. But when the liver is scarred from hepatitis, fatty liver, or alcohol damage, these factories don’t work right. The enzymes slow down. The clearance rate drops. And instead of being removed, the drug-and its toxic byproducts-stick around longer.
What Happens When the Liver Fails
In advanced liver disease, opioid half-lives can double, triple, or even multiply by six. For oxycodone, the normal half-life is about 3.5 hours. In someone with severe liver impairment, it can stretch to 14 hours on average, and in some cases, up to 24.4 hours. That means if you take a dose every 6 hours, by the third dose, you’re already carrying more than double the intended amount in your system.
Morphine is even more dangerous in this setting. Its metabolite M3G doesn’t get cleared properly, and levels can rise 3 to 5 times higher than normal. Studies show that patients with Child-Pugh Class C cirrhosis have up to a 70% reduction in morphine clearance. That’s not a small adjustment-it’s a red flag.
And it’s not just about the drug itself. The liver damage often comes with other problems: poor kidney function, fluid buildup, low protein levels-all of which change how opioids move through the body. The brain becomes more sensitive to opioids because the blood-brain barrier gets leaky. Even normal blood levels can cause extreme drowsiness, respiratory depression, or coma.
Which Opioids Are Riskiest in Liver Disease?
Not all opioids are created equal when it comes to liver damage. Some are far more dangerous than others.
Morphine is one of the worst choices. Because it relies entirely on glucuronidation, and that pathway gets overwhelmed in liver disease, it’s a ticking time bomb. Even early-stage cirrhosis calls for a 50% dose reduction. In severe cases, dosing intervals need to be stretched to every 12-24 hours.
Oxycodone is metabolized by two enzymes: CYP3A4 and CYP2D6. In liver failure, CYP3A4 activity drops by up to 60%. That means more of the drug stays active. Experts recommend starting at just 30%-50% of the normal dose and watching closely for sedation or breathing issues.
Methadone is tricky. It’s broken down by several CYP enzymes, so it might seem safer-but there are no clear dosing guidelines for liver disease. It also builds up in fat tissue and can linger for days. That makes it risky for long-term use in people with impaired livers.
Fentanyl and buprenorphine are better options, but not perfect. Fentanyl is metabolized by CYP3A4, so it’s still affected. But because it’s often given as a patch, it bypasses the liver’s first-pass metabolism. That’s a big advantage. Buprenorphine is mostly cleared by the liver too, but it has a ceiling effect-it doesn’t cause respiratory depression as easily at higher doses. Still, data is limited, and caution is needed.

How Liver Disease Changes the Rules for Dosing
There’s no one-size-fits-all dosing chart for opioids in liver disease. But here’s what works in practice:
- Start low. Use 30%-50% of the usual starting dose.
- Wait longer between doses. Don’t rush to increase frequency.
- Avoid long-acting formulations unless absolutely necessary.
- Monitor for sedation, confusion, slow breathing, and low blood pressure.
- Use the lowest effective dose for the shortest time possible.
For morphine: Reduce dose by 50% in mild liver disease. In severe disease, reduce dose by 75% and extend dosing to every 12-24 hours.
For oxycodone: Start at 2.5-5 mg every 8-12 hours instead of 5-10 mg every 6 hours.
Never assume a patient’s tolerance level. Someone who’s been on opioids for years with a healthy liver may not tolerate the same dose if their liver has failed.
Beyond Metabolism: How Opioids Can Worsen Liver Damage
The problem isn’t just that the liver can’t process opioids-it’s that opioids might make the liver worse.
Chronic opioid use changes the gut microbiome. It slows down gut movement, increases intestinal permeability, and lets toxins from the gut leak into the bloodstream. These toxins go straight to the liver, triggering inflammation. This is called the gut-liver axis, and it’s a major driver of progression in fatty liver disease and alcoholic liver disease.
Studies show that people on long-term opioids have higher levels of liver enzymes and more liver scarring over time-even without alcohol or hepatitis. The exact mechanism isn’t fully understood, but it’s clear: opioids aren’t just passive players. They can actively harm the liver.
What About Age, Gender, or Other Factors?
Age doesn’t change how CYP3A4 works. Neither does gender or ethnicity-though women do have slightly higher enzyme activity on average. That’s not enough to change dosing rules, but it’s a reminder that individual variation matters.
What does matter? The cause of liver disease. In alcohol-related liver disease, CYP2E1 becomes overactive, which can speed up metabolism of some drugs-but also create more toxic byproducts. In non-alcoholic fatty liver disease (NAFLD), CYP3A4 activity drops, making opioids stick around longer. So two people with cirrhosis might need completely different approaches based on what caused their liver damage.
What’s Still Unknown?
There are big gaps in our knowledge. We don’t have solid dosing guidelines for fentanyl, hydromorphone, or tramadol in liver disease. We don’t know how opioid-induced liver injury compares across different types of liver disease. We don’t know if switching from oral to transdermal opioids reduces long-term liver damage.
Most studies are small, retrospective, or based on animal models. Large, controlled trials in people with advanced liver disease are rare. That means doctors often have to guess.
That’s why guidelines from the American Association for the Study of Liver Diseases (AASLD) and the World Health Organization (WHO) stress caution: avoid opioids if possible. Use non-opioid pain relievers first. Try physical therapy, nerve blocks, or antidepressants for chronic pain. If opioids are necessary, start low, go slow, and monitor constantly.
What Should Patients Do?
If you have liver disease and are on opioids:
- Ask your doctor: Is this the safest opioid for my liver condition?
- Ask: Can we try a non-opioid option first?
- Report any new dizziness, confusion, or trouble breathing immediately.
- Don’t take extra doses-even if you feel the pain is coming back.
- Keep a pain and medication journal. Note timing, dosage, and side effects.
If you’re a caregiver, watch for signs of overdose: slow or shallow breathing, blue lips, unresponsiveness. Keep naloxone on hand if opioids are being used at home.
There’s no perfect solution. But understanding how liver disease changes opioid metabolism is the first step toward safer care. It’s not about avoiding pain relief-it’s about getting it without risking your life.
Can opioids cause liver damage on their own?
Yes, though not directly like acetaminophen. Chronic opioid use can worsen liver disease by disrupting the gut microbiome, increasing gut permeability, and allowing bacterial toxins to reach the liver. This triggers inflammation and can speed up scarring, especially in fatty liver or alcohol-related liver disease. It’s an indirect but real risk.
Is codeine safe for people with liver disease?
No. Codeine is converted to morphine by the CYP2D6 enzyme. In liver disease, this conversion becomes unpredictable-some people make too much morphine, others too little. That makes dosing unreliable and increases overdose risk. It’s generally avoided in people with liver impairment.
Why is morphine riskier than fentanyl in liver disease?
Morphine depends on glucuronidation, a pathway that shuts down early in liver disease. Its toxic metabolite, M3G, builds up quickly. Fentanyl is metabolized by CYP3A4, which also declines-but when given as a patch, it bypasses the liver entirely. That makes transdermal fentanyl a safer option in many cases.
Can I use ibuprofen or acetaminophen instead of opioids for pain?
Ibuprofen can be risky in advanced liver disease because it affects kidney function and increases bleeding risk. Acetaminophen is safer in low doses-up to 2,000 mg per day for most people with liver disease-but even that should be monitored. Neither is as strong as opioids for severe pain, but they’re better first-line choices when possible.
How often should liver function be checked if I’m on long-term opioids?
Every 3-6 months if you have stable liver disease. If your liver condition is worsening, check every 1-2 months. Blood tests for ALT, AST, bilirubin, and albumin help track both liver health and whether opioids might be adding stress. Always report new fatigue, yellowing skin, or swelling.
If you’re living with liver disease and need pain relief, you’re not alone. But you need a plan that’s tailored to your liver-not just your pain. The right approach means less risk, better control, and more quality time.
Abhi Yadav
November 30, 2025 AT 07:55Julia Jakob
December 1, 2025 AT 07:24Robert Altmannshofer
December 2, 2025 AT 16:56Kathleen Koopman
December 3, 2025 AT 00:50Nancy M
December 3, 2025 AT 04:35gladys morante
December 4, 2025 AT 06:08Precious Angel
December 6, 2025 AT 00:12Melania Dellavega
December 6, 2025 AT 21:58Bethany Hosier
December 8, 2025 AT 04:32Krys Freeman
December 9, 2025 AT 22:18Shawna B
December 10, 2025 AT 23:17Jerry Ray
December 11, 2025 AT 13:50David Ross
December 13, 2025 AT 12:40Sophia Lyateva
December 14, 2025 AT 08:41AARON HERNANDEZ ZAVALA
December 15, 2025 AT 17:25Lyn James
December 16, 2025 AT 22:16Rachel Nimmons
December 17, 2025 AT 08:38