Over half of adults will deal with hemorrhoids by the time they turn 50. That’s not rare. It’s normal. But knowing whether to reach for an OTC cream or call a doctor can feel confusing-especially when your butt is burning, itching, or bleeding. You’re not alone if you’ve stared at the pharmacy shelf, wondering if Preparation H will fix this or if you’re just wasting money.
What OTC Hemorrhoid Treatments Actually Do
OTC hemorrhoid treatments don’t cure hemorrhoids. They don’t shrink swollen veins or fix the root cause. What they do is give you temporary relief-usually for a few hours at a time. Think of them like a bandage on a cut: they help you feel better while your body heals, but they don’t heal the cut itself.
There are four main types of active ingredients in these products:
- Local anesthetics like benzocaine or pramoxine numb the area. They work fast-within minutes-and last 2 to 4 hours. Good for sudden pain or itching.
- Astringents like witch hazel (usually 14% concentration) tighten tissue and reduce swelling. Tucks pads are the most common. They give instant cooling relief but wear off in 30 to 60 minutes.
- Vasoconstrictors like phenylephrine (0.25% in Preparation H) shrink blood vessels. This reduces puffiness and discomfort. It kicks in within 15 minutes but fades quickly.
- Corticosteroids like hydrocortisone (1%) reduce inflammation. But here’s the catch: they take 3 to 4 days of consistent use before you notice any difference. Don’t give up after one application.
Suppositories are better for internal hemorrhoids. A 25mg hydrocortisone suppository, inserted after a bowel movement, gives relief directly where it’s needed. Studies show 87% of users feel better within 48 hours when used correctly.
Which Product Works Best for Your Type
Not all hemorrhoids are the same. Your treatment should match your symptoms.
External hemorrhoids (swollen lumps outside the anus) respond best to creams and wipes. Witch hazel pads give quick, soothing relief. Benzocaine creams block pain longer. A 2021 study found that combination products-like Anusol HC, which has both pramoxine and hydrocortisone-are 40% more effective than single-ingredient options.
Internal hemorrhoids (inside the rectum) are harder to reach. Creams don’t stick well. Suppositories work better. The Mayo Clinic recommends inserting them right after you go to the bathroom, when the rectum is empty. This helps the medicine absorb properly. If you use them too early or too late, effectiveness drops by 35%.
For mild swelling and irritation, zinc oxide or Calmoseptine creams are gentle, non-medicated options. They don’t numb or shrink-you’re just protecting the skin. They’re safe for daily use and won’t irritate sensitive skin.
When OTC Treatments Don’t Work (And Why)
Here’s the hard truth: OTC treatments fail for about 1 in 4 people. Not because they’re weak. Because the problem is too advanced.
Grade I and II hemorrhoids-those that bleed a little or bulge slightly but go back in on their own-are the only ones that respond well to OTC care. Once you’re dealing with grade III or IV (hemorrhoids that prolapse and won’t go back in), creams and suppositories won’t cut it. NIH data shows only 15% of people with these advanced cases see any improvement with OTC products. The rest need medical procedures like rubber band ligation, which works 95% of the time.
Another big reason OTC treatments fail? People use them wrong.
- Applying too often: 42% of users apply more than the recommended 3-4 times per day. This can irritate skin, not help it.
- Stopping too soon: 68% quit after 3 days. But hydrocortisone needs 3-4 days just to start working. Give it 7-14 days.
- Not cleaning the area: If you don’t wash and dry the area before applying, the medicine can’t stick. Tampa Colorectal Specialists found improper hygiene cuts effectiveness by 65%.
- Storing it wrong: Some creams need refrigeration. Leaving them on the counter can break down the active ingredients.
And yes-some products just don’t work for you. Amazon reviews for Tucks show 73% of 5-star ratings say “instant cooling relief.” But 41% of negative reviews on hydrocortisone creams say “no improvement after 7 days.” That’s not a flaw in the product. It’s a mismatch between the treatment and the problem.

What You Should Do Right Now
Here’s your simple action plan:
- Use witch hazel pads or a cream with benzocaine for immediate relief from itching or burning.
- If you have internal discomfort or bleeding, try a hydrocortisone suppository after each bowel movement.
- Take warm sitz baths-15 to 20 minutes, 2-3 times a day. It reduces swelling and helps healing.
- Keep the area clean and dry. Use unscented wipes or gentle soap. No harsh toilet paper.
- Don’t strain. Drink water. Eat fiber. Avoid sitting too long.
Track your symptoms. Write down what you’re using, when, and how you feel after. That helps you-and your doctor-see what’s working.
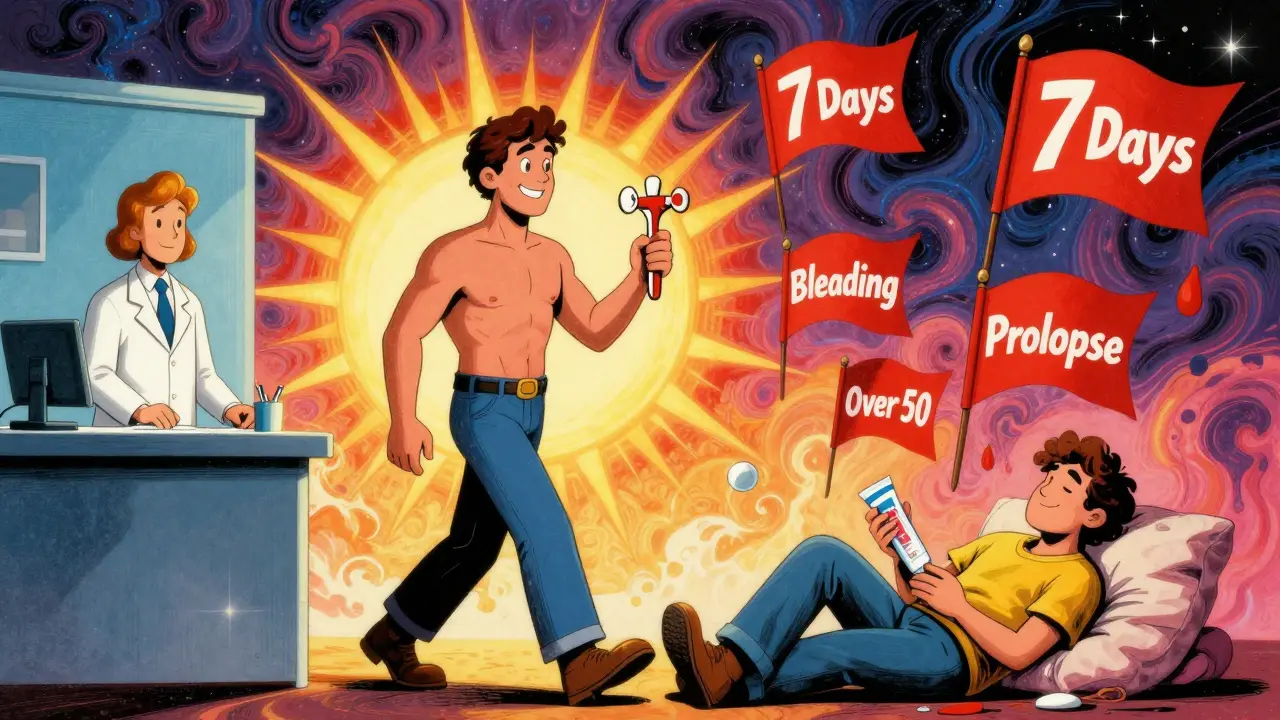
When to Call a Doctor
You don’t need to suffer for weeks. There are clear red flags:
- Symptoms last longer than 7 days, even with proper OTC use.
- You see bright red blood in your stool or on the toilet paper. This isn’t always hemorrhoids-could be something more serious.
- You feel a painful lump that won’t go back in.
- Pain is severe, constant, or getting worse.
- You’re over 50 and this is your first time having symptoms. New rectal bleeding at that age needs checking.
Doctors have stronger options: 2.5% hydrocortisone creams, prescription suppositories, or quick in-office procedures like rubber band ligation. These aren’t scary. They’re fast. Most take less than 15 minutes. Recovery is usually a few days.
Waiting too long is the biggest mistake. Tampa Colorectal Specialists found 82% of patients who needed medical care waited longer than they should. By then, the problem is harder to fix-and more expensive.
What’s Coming Next
The OTC market is growing fast. Sales hit $1.2 billion in 2022 and are expected to hit $1.8 billion by 2027. But the real change is coming from science.
New treatments are in development: sustained-release suppositories that last 12 hours, nanoemulsion creams that penetrate deeper, and even therapies targeting the root cause-swollen veins-not just the symptoms. These aren’t on shelves yet, but they’re coming.
Right now, the best thing you can do is treat smart. Use OTC products correctly. Don’t delay care. And know this: hemorrhoids are common, treatable, and rarely dangerous. But they won’t fix themselves. You have to act.
Can I use OTC hemorrhoid treatments every day?
Yes, but only for up to 7 days. Most creams and suppositories are designed for short-term use. Using hydrocortisone for longer than 7 days can thin your skin or cause other side effects. Witch hazel and zinc oxide are gentler and can be used longer, but if symptoms persist beyond a week, see a doctor.
Is Preparation H better than witch hazel?
It depends on your symptoms. Preparation H (with phenylephrine) is best for reducing swelling and puffiness. Witch hazel is better for soothing itching and burning. If you have both issues, try using witch hazel pads in the morning and Preparation H at night. Combination products like Anusol HC work well for mixed symptoms.
Why do some people say OTC treatments don’t work?
Because they’re using them for the wrong reason. OTC products relieve symptoms-they don’t fix the underlying problem. If your hemorrhoids are grade III or IV, no cream will make them go away. Also, many people stop using them too soon, apply them incorrectly, or don’t pair them with lifestyle changes like fiber and hydration. That’s why 47% of people who start with OTC treatments end up seeing a doctor within two weeks.
Can hemorrhoids go away on their own?
Mild cases (grade I-II) often improve within a few days to a week with proper care-hydration, fiber, sitz baths, and OTC treatments. But they don’t disappear forever. The veins stay weak. Without lifestyle changes, they’ll likely come back. Severe cases (grade III-IV) won’t resolve without medical treatment.
Is rectal bleeding always from hemorrhoids?
No. Bright red blood on toilet paper or in the toilet can be from hemorrhoids, but it can also signal anal fissures, colon polyps, or even colorectal cancer. If you’re over 50, have a family history of colon issues, or the bleeding is heavy, dark, or accompanied by weight loss or changes in bowel habits, see a doctor immediately. Don’t assume it’s just hemorrhoids.
What to Do Next
If you’re using OTC treatments and feeling better, keep going-but don’t ignore the warning signs. If you’re still in pain after a week, or if bleeding happens again, don’t wait. Make an appointment. You don’t need to feel embarrassed. Doctors see this every day. The sooner you act, the less invasive the fix will be.
And if you’re not sure what’s going on? Take a photo of the area (yes, really). Show it to your doctor. It helps more than you think. Most people feel better within days once they get the right treatment. You don’t have to live with it.

kenneth pillet
January 18, 2026 AT 17:50Been using witch hazel pads for years. Works like a charm if you don’t overdo it. Just wipe, don’t rub. Dry good. No more burning.
Simple.
Dayanara Villafuerte
January 19, 2026 AT 01:14OTC creams are basically the placebo effect with extra steps 😅
Witch hazel = instant chill vibes.
Hydrocortisone? Wait 3 days? Bro, I’m not that patient. 🤷♀️
Also, sitz baths are underrated. I turn my tub into a spa. Candles optional but recommended. 🕯️
Andrew Qu
January 20, 2026 AT 16:55Good breakdown. A lot of people don’t realize hydrocortisone takes days. I tell my patients: treat it like a muscle injury - rest, consistency, patience. No magic sprays.
And yes - hygiene matters more than you think. Wipe gently. Pat dry. No rough TP. Your butt will thank you.
Also, fiber. Eat it. Like, actually eat it. Psyllium husk is your new BFF.
Jodi Harding
January 21, 2026 AT 21:32They sell these like candy. But the body doesn’t heal with chemicals - it heals with rest, hydration, and not sitting on a toilet for 20 minutes scrolling TikTok.
Stop treating symptoms. Start treating habits.
Naomi Keyes
January 23, 2026 AT 19:46Actually, the data on hydrocortisone efficacy is misleading - most studies are industry-funded, and the 87% figure? That’s from a single, small, non-blinded trial with no placebo control. Also, suppositories are not FDA-regulated as strictly as creams - many contain undisclosed fillers. You’re essentially injecting unknown compounds into your rectum. Think about that.
Danny Gray
January 24, 2026 AT 03:25So we’re told to use these products - but who really benefits? The pharmaceutical industry? The pharmacy chains? The people who sell Tucks on Amazon Prime? Or the patient?
Let’s be real - this is capitalism disguised as healthcare.
And yet, we’re told to ‘take responsibility’ for our health… while being sold a $12 tube of magic jelly.
Tyler Myers
January 25, 2026 AT 08:55They don’t want you to know this - but hemorrhoids are a side effect of sitting on government-mandated chairs. All those ergonomic office chairs? Designed by Big Pharma to keep you seated. The real cure? Stand-up desks. Or better yet - squat toilets. That’s what they used in ancient Rome. They didn’t have hemorrhoids then. Coincidence? I think not.
rachel bellet
January 26, 2026 AT 14:36Let’s deconstruct the clinical terminology: vasoconstrictors induce transient ischemia - which is essentially a controlled micro-infarction of the hemorrhoidal plexus. That’s not healing. That’s vascular suppression. And corticosteroids? They downregulate IL-6 and TNF-alpha pathways - which is immunosuppressive. You’re not curing inflammation. You’re masking it with systemic immunomodulation. And you’re doing it for 7 days? That’s a recipe for epithelial atrophy. This isn’t treatment. It’s a pharmacological Band-Aid on a ruptured artery.
Ryan Otto
January 28, 2026 AT 02:48One must question the epistemological foundations of OTC medicine. If the mechanism of action is purely symptomatic - and the root pathology remains unaddressed - then we are engaging in a form of therapeutic nihilism disguised as self-care. The proliferation of these products reflects a societal aversion to discomfort, not a genuine commitment to health. One does not heal by numbing pain. One heals by confronting the conditions that generate it - poor diet, sedentary behavior, and the commodification of bodily suffering.
Robert Cassidy
January 30, 2026 AT 00:59They’re lying to you. They want you to think it’s just hemorrhoids. But it’s not. It’s the system. The government doesn’t want you to know that hemorrhoids are caused by GMO fiber additives. They’re designed to inflame your colon so you buy more creams. The real solution? Raw, organic, unprocessed flaxseed - imported from Canada. Not the U.S. They’re in on it. Also, avoid toilet paper. Use a bidet. Or your hand. But wash it with soap. And don’t trust the FDA.
Zoe Brooks
January 30, 2026 AT 06:34My grandma used to say, ‘If your butt’s mad, feed it broccoli and sit in warm water.’
Turns out, she was right.
And she never owned a single OTC cream.
She lived to 94.
Just saying.
Kristin Dailey
January 30, 2026 AT 13:03America’s healthcare system is broken. But you know what’s worse? People wasting money on creams instead of fixing their diet. Get real. Eat real food. Stop being lazy.
Chuck Dickson
January 30, 2026 AT 20:31Hey - if you’re reading this and you’ve got hemorrhoids? You’re not alone. And you’re not gross. This happens to everyone - even your favorite fitness influencer. I’ve been there. I used witch hazel, sat in warm water, ate a pound of beans a day, and didn’t sit for 3 hours straight. It took 5 days. Not magic. Just consistency.
You got this. And if it doesn’t get better? Go see a doctor. No shame. We’ve all been there. Seriously.
Max Sinclair
January 31, 2026 AT 20:33Thank you for writing this with such clarity. Too many posts either oversimplify or terrify. This strikes the right balance - practical, evidence-based, and compassionate.
Also, the point about hygiene cutting effectiveness by 65%? That’s critical. I never realized how much dirt and moisture were interfering with absorption.
Worth sharing with everyone I know.
Aysha Siera
February 1, 2026 AT 21:58They say it’s hemorrhoids. But I think it’s the 5G towers. They’re targeting the lower GI tract. I stopped using WiFi and started sleeping on copper sheets. The burning stopped. Coincidence? I think not.