Many people turn to St. John’s Wort because they want a "natural" way to manage mild depression. It’s available over the counter, often marketed as safe and gentle. But here’s the hard truth: if you’re taking any prescription medication, St. John’s Wort could be quietly sabotaging your treatment - and you might not even know it.
How St. John’s Wort Changes How Your Body Handles Medication
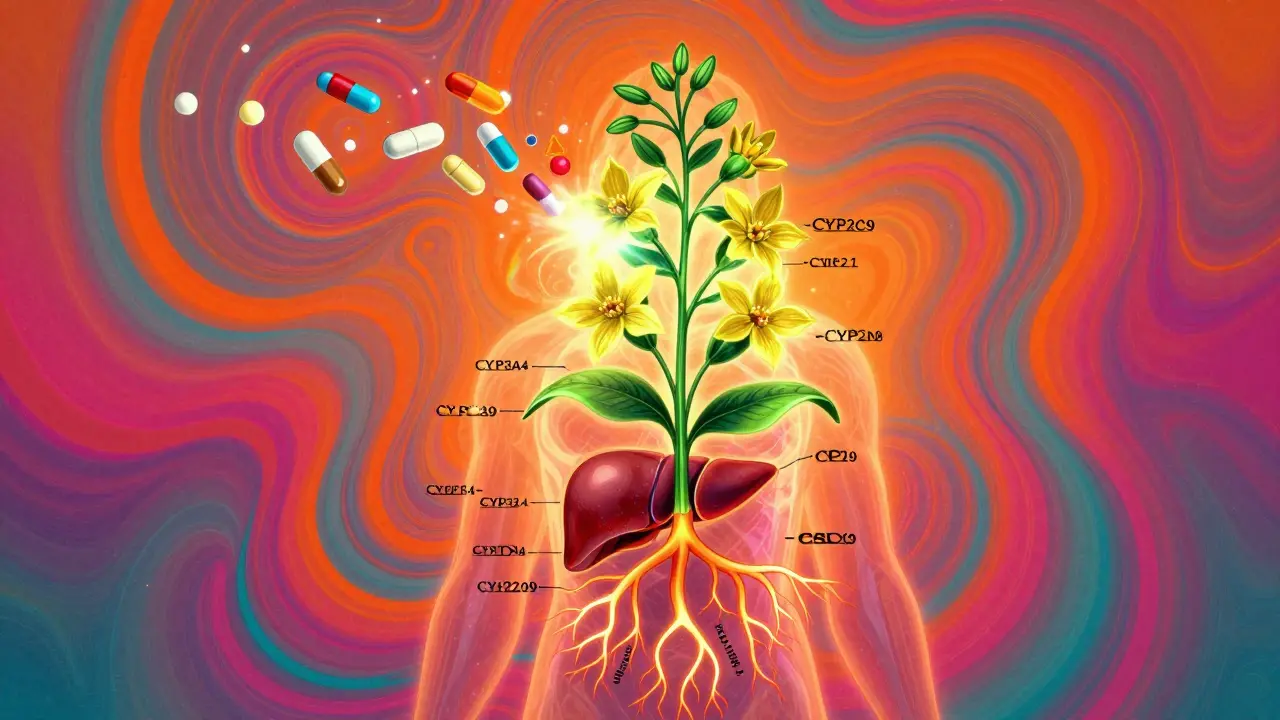
St. John’s Wort doesn’t just sit in your system. It actively rewires how your body processes drugs. The key player is a compound called hyperforin. This one ingredient triggers your liver to ramp up production of enzymes - especially CYP3A4 and CYP2C9 - that break down medications. At the same time, it boosts P-glycoprotein, a transporter that pushes drugs out of your cells faster.
The result? Your body clears drugs like they’re going out of style. Studies show St. John’s Wort can slash blood levels of certain medications by 30% to 50%. That’s not a minor drop. For drugs with narrow safety windows - like blood thinners or transplant meds - even a 20% change can be dangerous.
And here’s the kicker: these effects don’t disappear when you stop taking St. John’s Wort. Because your liver keeps producing those enzymes for weeks, the interaction can last up to two weeks after you quit. That means even if you stop the herb before starting a new drug, you’re not safe.
Drugs That Can Fail - Or Turn Dangerous - With St. John’s Wort
St. John’s Wort doesn’t play favorites. It messes with a long list of critical medications. Here are the most dangerous ones:
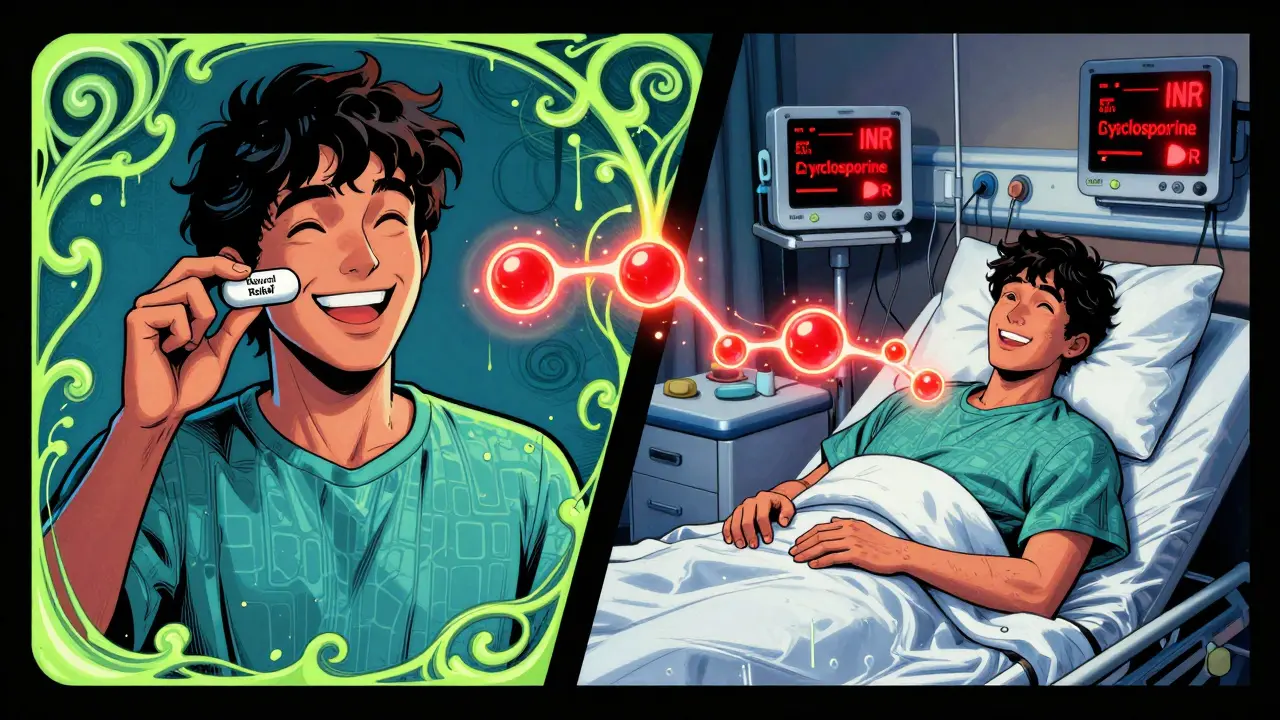
- Warfarin and other blood thinners: A 2023 review by the Therapeutic Goods Administration (TGA) documented 22 cases where patients on warfarin saw their INR levels plunge from therapeutic (2.0-3.0) to dangerously low (1.2-1.8) within days of starting St. John’s Wort. One patient’s INR dropped from 2.8 to 1.5 in just 10 days. That’s a ticking time bomb for clots, stroke, or pulmonary embolism.
- Birth control pills: Ethinyl estradiol, the hormone in most oral contraceptives, gets metabolized faster. The TGA and GoodRx both report 13 confirmed cases of unintended pregnancy despite perfect pill use. Breakthrough bleeding? That’s often the first warning sign.
- Immunosuppressants like cyclosporine: Organ transplant patients who took St. John’s Wort for depression saw cyclosporine levels drop by 30-50%. One patient shared online: "My doctor said I was hours away from rejection." This isn’t hypothetical - it’s life-or-death.
- HIV medications: Protease inhibitors like saquinavir and non-nucleoside reverse transcriptase inhibitors like efavirenz can lose up to 50% of their effectiveness. That means the virus can rebound, resistance can develop, and treatment can collapse.
- Antidepressants: St. John’s Wort itself boosts serotonin. If you’re already on an SSRI like sertraline or fluoxetine, you’re stacking two serotonin boosters. The TGA recorded six Australian cases of serotonin syndrome - a condition that can cause seizures, high fever, and even death.
- Anticonvulsants: Phenytoin and carbamazepine levels can drop by 30-40%. For someone with epilepsy, that’s a direct path to uncontrolled seizures.
- Benzodiazepines: Alprazolam (Xanax) levels can fall by 40%. Anxiety that was under control can return with a vengeance.
- Statins: Atorvastatin and simvastatin - two of the most common cholesterol drugs - lose 30-40% of their effect. Pravastatin and fluvastatin? They’re safer. But most people don’t know which is which.
- Digoxin, theophylline, and opioids: All show clinically significant drops in blood levels. Heart failure, asthma attacks, and loss of pain control are real risks.
Why People Don’t Realize They’re at Risk
Most users think herbal means harmless. A 2022 Johns Hopkins study found that 41% of people taking prescription drugs didn’t tell their doctor they were using St. John’s Wort. Why? Because they don’t see it as a "medication."
Pharmacists report the same pattern: patients will list every pill they take - but skip the little bottle labeled "herbal supplement." And even when they do mention it, many doctors don’t ask. The question "Are you taking any other medications?" misses the mark. The right question is: "Do you take any herbal supplements, vitamins, or non-prescription products?"
Online reviews add to the confusion. On WebMD, 68% of users say St. John’s Wort worked wonders for their depression. But those stories rarely mention the warfarin they’re on, or the birth control they’re using. The risks are invisible in the testimonials.
What You Should Do - If You’re Taking St. John’s Wort
If you’re using St. John’s Wort and take any prescription drugs, here’s what to do right now:
- Stop taking it immediately - and don’t restart until you’ve talked to your doctor.
- Check every medication. Don’t guess. If you’re on any of the drugs listed above, assume there’s an interaction.
- Ask for testing. For warfarin, get an INR check within 3-5 days of stopping. For cyclosporine, ask for a trough level. For birth control, consider switching to a non-hormonal method.
- Wait two weeks before starting any new medication. Your liver needs time to reset.
There’s no safe gray area. The European Food Safety Authority says it plainly: "No safe threshold can be established." Even low doses, even short use - it all adds up.
What’s Changing in the Medical World
Regulators are catching up. In Australia, all St. John’s Wort products must carry a warning about drug interactions. The FDA now requires labels to say: "Ask a doctor before use if you are taking prescription drugs." The Institute for Safe Medication Practices added it to their 2023 list of high-alert herbal products - the same category as insulin and heparin.
Some researchers are exploring ways to make it safer. A 2023 study in Clinical Pharmacology & Therapeutics found that extracts with less than 0.3% hyperforin had far fewer interactions - while still helping with mood. But these aren’t available on store shelves yet.
And the medical community is shifting. The American Psychiatric Association’s 2023 guidelines no longer say "may be considered" for depression. They now say: "Not recommended for patients taking any prescription medications."

Bottom Line
St. John’s Wort isn’t a harmless herb. It’s a powerful enzyme inducer with the ability to turn life-saving drugs into useless ones. The benefits for mild depression are real - but they come with a price tag most people never see: hospital visits, organ rejection, unplanned pregnancies, strokes, seizures.
If you’re considering it - or already using it - talk to your doctor. Not your friend. Not your pharmacist. Not Google. Your doctor. Bring the bottle. Show them the label. Ask: "Could this interfere with my other meds?"
"Natural" doesn’t mean safe. It just means unregulated. And right now, that’s a gamble you can’t afford to take.
Can I take St. John’s Wort with antidepressants?
No. St. John’s Wort increases serotonin levels in the brain. When taken with SSRIs, SNRIs, or other antidepressants like nefazodone, it can cause serotonin syndrome - a dangerous condition with symptoms like confusion, rapid heart rate, high blood pressure, fever, tremors, and seizures. The Therapeutic Goods Administration (TGA) has documented six cases in Australia alone. Even if you feel fine, the risk is real and can escalate quickly.
How long does St. John’s Wort stay in my system?
The active compound hyperforin can keep your liver enzymes turned on for up to two weeks after you stop taking it. That means even if you quit the herb, your body will still process other medications faster during that time. This is why doctors recommend a minimum 2-week washout period before starting drugs like warfarin, cyclosporine, or birth control pills.
Are all St. John’s Wort supplements the same?
No. The amount of hyperforin varies widely between brands - and most labels don’t list it. Standardized extracts with 0.3% hyperforin show less interaction in studies, but they’re rare in stores. Most over-the-counter products contain 0.5% to 3% hyperforin - enough to trigger dangerous enzyme induction. You can’t rely on brand reputation or "natural" labels to keep you safe.
Can I take St. John’s Wort if I’m not on any meds?
If you’re not taking any prescription drugs, over-the-counter medications, or even birth control, the risk of interaction is low. But that doesn’t mean it’s risk-free. St. John’s Wort can still cause side effects like dry mouth, dizziness, or increased sun sensitivity. And if you start taking any medication later - even an antibiotic or painkiller - you could trigger an interaction. It’s safer to avoid it entirely unless under medical supervision.
Why don’t more doctors warn patients about this?
Many don’t ask. Surveys show that 73% of patients experiencing harmful interactions weren’t asked about herbal supplements. Doctors often assume patients will volunteer the information - but most don’t consider supplements "medications." The American Academy of Family Physicians recommends asking: "Do you take any herbal supplements, vitamins, or non-prescription medicines?" - not just "Are you taking any other medications?" If your doctor doesn’t ask, speak up.
Is there a safer alternative for depression?
Yes. For mild depression, evidence supports regular exercise, cognitive behavioral therapy (CBT), and certain SSRIs with lower interaction risks - like escitalopram or sertraline - when monitored properly. Light therapy and mindfulness practices also show benefit. Unlike St. John’s Wort, these options don’t interfere with other medications and have well-documented safety profiles. Talk to your doctor about what’s right for you - without relying on unregulated supplements.
Next Steps
If you’re currently taking St. John’s Wort and any prescription drugs:
- Stop the supplement immediately.
- Call your doctor or pharmacist. Bring the product label.
- Ask: "Could this have affected my other medications?" and "Do I need any tests?"
- If you’re on warfarin, birth control, or immunosuppressants - get a blood test within the next week.
- Don’t restart without medical approval.
If you’re thinking about starting St. John’s Wort:
- Don’t. Not unless your doctor has reviewed every medication you take - and approved it.
- There are safer, regulated options for depression that don’t come with hidden risks.
- Your health isn’t worth the gamble.