Ever taken a pill and wondered if you should’ve eaten first? Or maybe you forgot, took it on an empty stomach, and ended up with nausea, dizziness, or just felt like it didn’t work? You’re not alone. Around 40% of prescription medications come with specific instructions about food - and getting it wrong can mean the difference between healing and harm.
Why Food Matters More Than You Think
It’s not just about avoiding an upset stomach. What you eat - or don’t eat - when you take your medicine changes how your body absorbs it. Food affects stomach acid, bile flow, how fast your stomach empties, and even the enzymes in your gut that break down drugs. These aren’t small tweaks. They can cut absorption in half or boost it by 40%. For example, the HIV drug saquinavir gets absorbed up to 40% better when taken with a high-fat meal. But take it with grapefruit juice? That can spike levels even higher, raising the risk of dangerous side effects. On the flip side, tetracycline and doxycycline bind to calcium in dairy, reducing absorption by up to 50%. That means your antibiotic might as well be water.Medications That Need Food
Some drugs simply don’t work right without food. Here’s what you should take with a meal:- NSAIDs like ibuprofen, naproxen, and aspirin: Food protects your stomach lining. While some older studies questioned the benefit, major health agencies - including the UK’s NHS and German medical guidelines - still recommend taking these with food, especially for older adults or those with a history of ulcers.
- Antibiotics like Augmentin (amoxicillin/clavulanate), Macrobid, and Mycobutin: Taking these with food cuts nausea by 20% and helps the drug stay active longer - up to 2 hours instead of just 20 minutes.
- Antiretrovirals like ritonavir and zidovudine: Food reduces nausea and vomiting. One Reddit user reported that taking ritonavir with a small peanut butter sandwich dropped nausea from 45% to 18%.
- Some cholesterol and blood pressure meds: Certain statins and beta-blockers are better absorbed with food, leading to more stable blood levels.
It’s not just about the meal - it’s about the type. High-fat meals boost absorption of fat-soluble drugs. A banana or toast might help with nausea, but it won’t do the same job as avocado or nuts for certain HIV meds.
Medications That Must Be Taken on an Empty Stomach
Other drugs are ruined by food. Taking them with a meal can make them useless - or worse, toxic.- Levothyroxine (for hypothyroidism): Food can slash absorption by 20% to 55%. That means your thyroid levels stay off, and you keep feeling tired, cold, or gaining weight. Take it 30 to 60 minutes before breakfast - and wait at least 4 hours before taking calcium, iron, or antacids.
- Tetracycline and doxycycline: Avoid dairy, antacids, and even calcium-fortified orange juice. These bind to the drug and block absorption.
- Didanosine (an older HIV drug): Stomach acid destroys it. Take it on an empty stomach, 30 minutes before or 2 hours after eating.
- Bisphosphonates like alendronate (Fosamax): These osteoporosis drugs need to be taken with a full glass of water, first thing in the morning, before any food or drink - even coffee. Lie down for 30 minutes after to avoid esophageal irritation.
Timing matters. The Mayo Clinic recommends taking empty-stomach meds either 1 hour before a meal or 2 hours after. For bisphosphonates, that window stretches to 30-60 minutes.
What About Grapefruit Juice?
Grapefruit juice isn’t just a breakfast staple - it’s a drug interaction wildcard. It blocks an enzyme in your gut called CYP3A4 that normally breaks down certain medications. That means more drug enters your bloodstream than intended. This affects:- Some statins (simvastatin, lovastatin)
- Some blood pressure meds (nifedipine, felodipine)
- HIV drugs like saquinavir
- Some anti-anxiety meds
Even one glass can cause effects that last over 24 hours. If your prescription says “avoid grapefruit,” it’s not a suggestion - it’s a safety rule.
Why Do Guidelines Sometimes Conflict?
You might read one source saying NSAIDs should be taken with food, and another saying it doesn’t matter. That’s because science evolves. A 2015 review in Inflammopharmacology found no strong proof that food prevents NSAID stomach damage - and suggested taking them on an empty stomach for faster pain relief. But the NHS and other agencies still recommend food, especially for high-risk patients. Why? Because real-world harm outweighs theoretical speed. A stomach ulcer is worse than 10 minutes of delayed pain relief. Dr. Alissa Keillor, a pharmacist at Parkview Health, puts it simply: “Food can change how your body responds to certain medications.” That’s why you need to follow your prescription label - not a blog post or your friend’s advice.Real People, Real Mistakes
A 2023 GoodRx survey of 5,000 people found that 42% admitted to taking their meds incorrectly regarding food. The worst offenders? People managing five or more prescriptions. One user on Reddit’s r/Pharmacy said they mixed up their levothyroxine and ibuprofen - took the thyroid med after breakfast, and the NSAID before. Result? Fatigue, weight gain, and stomach pain. It took three doctor visits to untangle. Another shared that they started taking their HIV meds with a banana instead of a full meal - and their viral load spiked. Turns out, bananas don’t have enough fat to trigger the right absorption.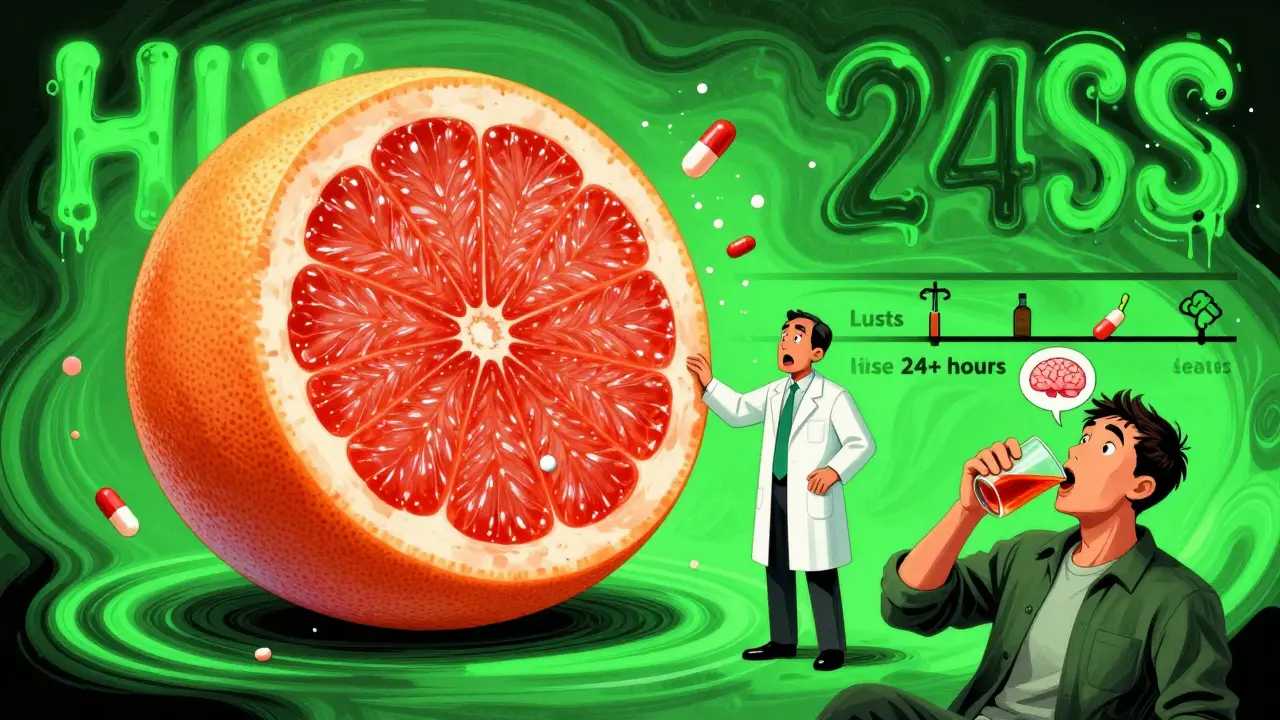
How to Get It Right Every Time
You don’t need to memorize a 10-page chart. Here’s how to make food and meds work for you:- Read the label - not just the name, but the fine print. “Take with food” or “take on empty stomach” is there for a reason.
- Ask your pharmacist - they’re trained to catch these details. In a 2024 Express Scripts report, patients who got clear food instructions from pharmacists had 27% higher adherence.
- Use color-coded labels - some pharmacies now use red for “empty stomach,” green for “with food,” and yellow for “with high-fat meal.”
- Set phone alarms - one Reddit user said they got 68% better at remembering with alarms labeled “Take med - no food for 1 hour.”
- Keep a simple log - write down what you took, when, and with what. It helps spot patterns if side effects pop up.
And don’t underestimate the power of knowing why. The American Pharmacists Association found that patients who understood the reason behind food rules were 44% more likely to stick to them.
What’s Changing in 2026?
The FDA just updated its 2024 draft guidance: drug labels can no longer just say “with or without food.” They now need to specify:- Meal size (light, regular, high-fat)
- Exact timing windows (e.g., “take 30 minutes before breakfast”)
- Food to avoid (e.g., “avoid dairy for 2 hours”)
Researchers are even testing personalized approaches. A 2024 UCSF study used gut microbiome tests to predict how someone’s body will respond to food-drug interactions - with 87% accuracy in early trials.
Meanwhile, hospitals are now required to include food instructions in discharge counseling - up from 76% in 2019 to 92% in 2024. That’s because mistakes here aren’t just inconvenient. They lead to hospital readmissions, failed treatments, and avoidable side effects.
Final Tip: When in Doubt, Wait
If your label doesn’t say anything about food, or you’re unsure - wait. Take the pill with a glass of water on an empty stomach. Wait 30 minutes before eating. It’s safer than guessing.Your body doesn’t treat every pill the same. What you eat isn’t just fuel - it’s part of your medicine’s delivery system. Get it right, and your treatment works as it should. Get it wrong, and you’re playing Russian roulette with your health.
Can I take my medication with just a sip of water and a small snack?
It depends on the drug. For medications that need an empty stomach - like levothyroxine or tetracycline - even a small snack can interfere. A sip of water is fine, but anything else - even a cracker or a piece of candy - counts as food. For drugs that require food, a small snack might not be enough. High-fat meals are needed for some HIV drugs, and a banana won’t cut it. Always follow the label’s specific instructions.
What if I forget and take my pill with food when I shouldn’t have?
Don’t panic, but don’t just keep going. If you took a drug like levothyroxine or doxycycline with food, skip your next dose and wait until the next scheduled time. Don’t double up. For drugs that need food, like NSAIDs, taking them without food once probably won’t cause serious harm - but it might reduce effectiveness or cause stomach upset. Call your pharmacist if you’re unsure. They can help you adjust without risking overdose or underdose.
Why do some pills say ‘take with food’ but my doctor says ‘take on empty stomach’?
This usually means the label is outdated or generic. Doctors sometimes adjust instructions based on your personal health, other meds, or how your body responds. Always follow your doctor’s advice - but bring the label to your next appointment. There may be a mismatch that needs updating. Pharmacists can also flag these conflicts in your electronic record.
Can I take my medication with coffee or tea?
Coffee and tea can interfere with some drugs. Coffee contains calcium and tannins that can bind to antibiotics like tetracycline or bisphosphonates. Green tea may affect how your liver processes certain heart and psychiatric meds. For empty-stomach meds, it’s best to wait 30-60 minutes after taking the pill before drinking coffee. For meds taken with food, black coffee is usually fine unless the label says otherwise. Always check with your pharmacist.
Are there any foods that help reduce side effects from meds?
Yes - but only for specific drugs. For NSAIDs, a banana or toast can ease stomach upset. For HIV meds like ritonavir, a small high-fat snack like peanut butter, cheese, or avocado reduces nausea significantly. For statins, eating a small amount of fiber-rich food can help with muscle aches. But these aren’t universal fixes. A food that helps one drug might block another. Always confirm with your pharmacist before using food to manage side effects.

Samyak Shertok
January 17, 2026 AT 18:44Stephen Tulloch
January 19, 2026 AT 06:45vivek kumar
January 21, 2026 AT 04:00Henry Ip
January 22, 2026 AT 18:24Isabella Reid
January 23, 2026 AT 23:43kanchan tiwari
January 25, 2026 AT 00:04Bobbi-Marie Nova
January 26, 2026 AT 19:51Allen Davidson
January 28, 2026 AT 06:09john Mccoskey
January 29, 2026 AT 07:25Joie Cregin
January 30, 2026 AT 20:57Rob Deneke
February 1, 2026 AT 10:35Chelsea Harton
February 2, 2026 AT 05:26Corey Chrisinger
February 3, 2026 AT 13:15Bianca Leonhardt
February 3, 2026 AT 20:59